Umbilical Cord Blood-derived Cell Therapy Promotes Remyelination in Mice
Written by |
A cell therapy product derived from human umbilical cord blood cells may be a promising treatment approach for patients with demyelinating diseases, such as multiple sclerosis (MS) or leukodystrophy, according to a recent study developed at the Duke University Medical Center.
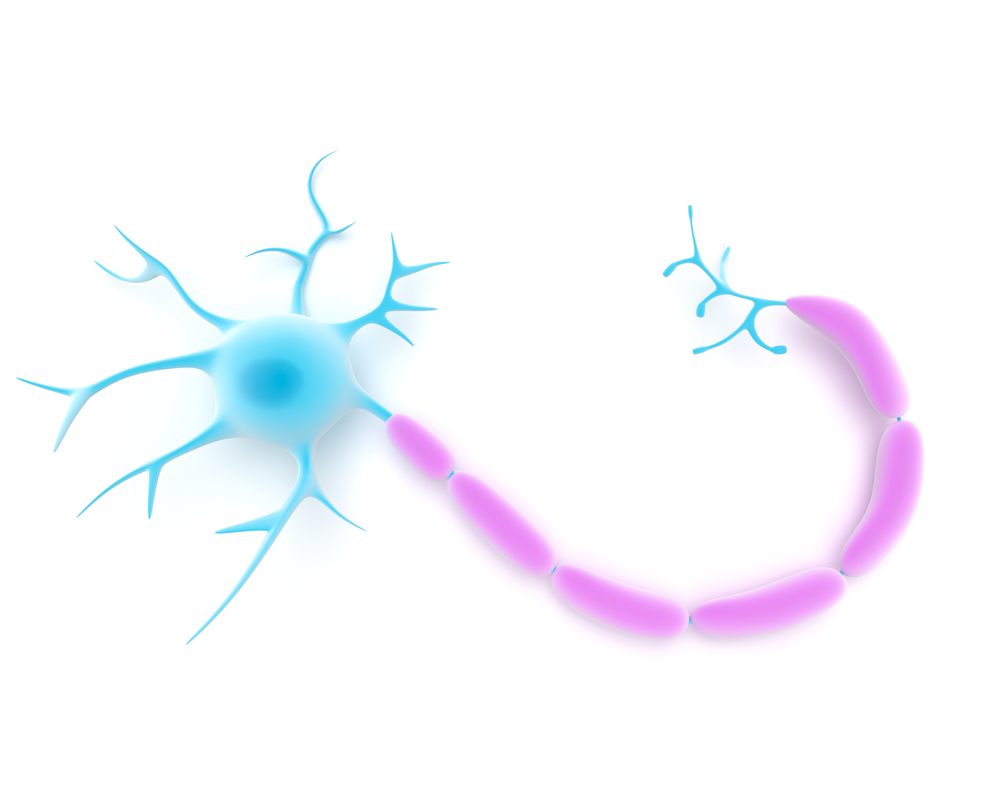
The study, “A cord blood monocyte–derived cell therapy product accelerates brain remyelination,” published in JCI Insight, shows that a cell product with characteristics of macrophages and microglia, the primary immune cells of the central nervous system (CNS), accelerated remyelination in mice subjected to toxic demyelination.
Microglia can exert a dual role in CNS injuries, participating in both their propagation and resolution, by modulating neuroinflammation, producing factors that regulate CNS cells, and clearing debris to provide an environment for oligondendrocytes (the myelin-producing cells) to remyelinate neurons.
Bone marrow-derived circulating blood monocytes have been proposed as a potential source of infiltrating immune cells that could exacerbate or ameliorate CNS damage. But there is limited information concerning the role of blood monocytes in the dynamics of brain injury repair, although studies have suggested that specific reparative monocyte populations, such as CD14-positive monocytes in human umbilical cord blood, could be considered as candidates for the treatment of injury-induced CNS demyelination.
Researchers used a cell product called DUOC-01 with characteristics of macrophages and microglia, and tested whether it would be useful in demyelinating diseases. DUOC-01 cells, which are derived of CD14-positive cells, are currently being evaluated in clinical trials for patients with pediatric leukodystrophy (a group of disorders characterized by the degeneration of white matter in the brain) in the setting of cord blood transplantation. Leukodystrophies lack specific enzymes, and the researchers here wanted proof-of-concept that DUOC-01 cells could be used in demyelinating diseases that do not arise from enzyme deficiency.
The team used DUOC-01 cells in mice with chemical-induced demyelination. They found that intracranially injected DUOC-01 induced rapid myelination, a higher proportion of fully myelinated neurons, and increased the differentiation of oligodendrocyte progenitor cells compared to uncultured cord blood CD14-positive macrophages.
“These studies constitute proof of concept that the monocyte-derived DUOC-01 cell product could provide benefit to patients with demyelinating conditions such as leukodystrophies, multiple sclerosis, or spinal cord injury,” the researchers wrote. “However, additional preclinical and early-phase clinical studies, based in part on the results presented here, will be necessary to bring this cell product to the clinic for treatment of such conditions.”


