FAQs about types of MS
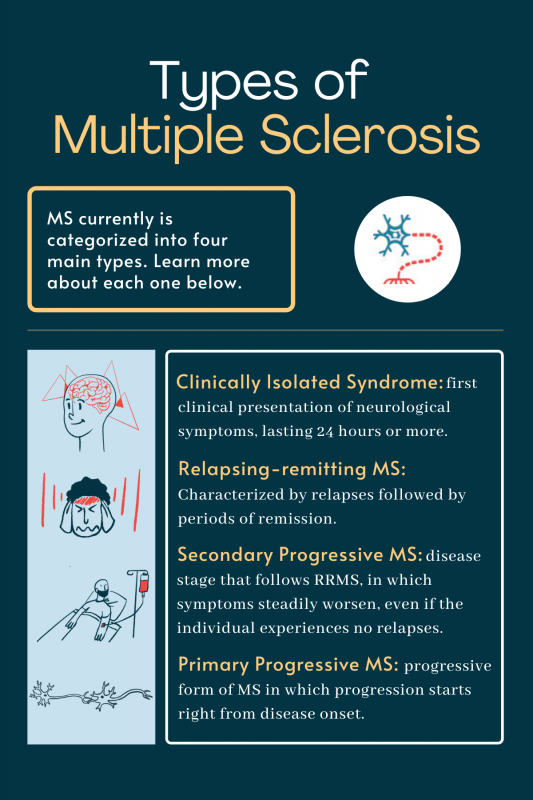
In general, progressive forms of multiple sclerosis, specifically primary progressive or secondary progressive MS, are associated with faster disease progression. That quicker progression results in a more rapid accumulation of disabling symptoms. However, the disease’s course is unique in every individual, and some patients with relapsing forms of MS may progress faster and experience more severe symptoms than someone with progressive forms ever will.
While multiple sclerosis affects everyone differently, patients with relapsing-remitting multiple sclerosis (RRMS) tend to experience a slower accrual of disabling symptoms than those with progressive forms. RRMS patients also experience remissions, or periods between exacerbations where symptoms disappear or ease considerably. In particular, mild RRMS is sometimes described as “benign” or “inactive” MS because of the lack of symptoms.
All forms of multiple sclerosis may cause symptoms that make some activities of daily life harder to do independently. In general, disability progression occurs more rapidly in progressive than relapsing forms of the disease, but there is substantial variation in progression patterns from person to person.
The most common form of multiple sclerosis is relapsing-remitting disease, or RRMS. About 85% of patients are first diagnosed with this MS type.
Actress Selma Blair, TV talk show host Montel Williams, and Ann Romney, author and the wife of Utah senator Mitt Romney all were initially diagnosed with relapsing-remitting multiple sclerosis, the most common form of the disease, in which periods of worsening symptoms (relapses) are interspersed by remissions when symptoms ease.
Related Articles

 Fact-checked by
Fact-checked by