University at Buffalo to Do Cognitive Training and Myelin Repair Studies
Written by |
University at Buffalo researchers are working on ways to improve multiple sclerosis patients’ cognitive function and to repair damage to the mylein coating that protects nerve cells.
The National Multiple Sclerosis Society awarded the researchers more than $1.1 million to conduct the studies.
One, “The Effects of Working Memory Training on Brain Function, Structure, and Cognition in MS,” will look at whether two neuroscience-based training programs can improve MS patients’ cognitive function. The MS society provided $609,000 for the three-year project.
The training programs will focus on improving patients’ working memory and processing speed. Both are impaired in people with MS.
Working memory is short-term process important to reasoning and decision-making. Processing speed is the time the brain needs to process information and formulate a response.
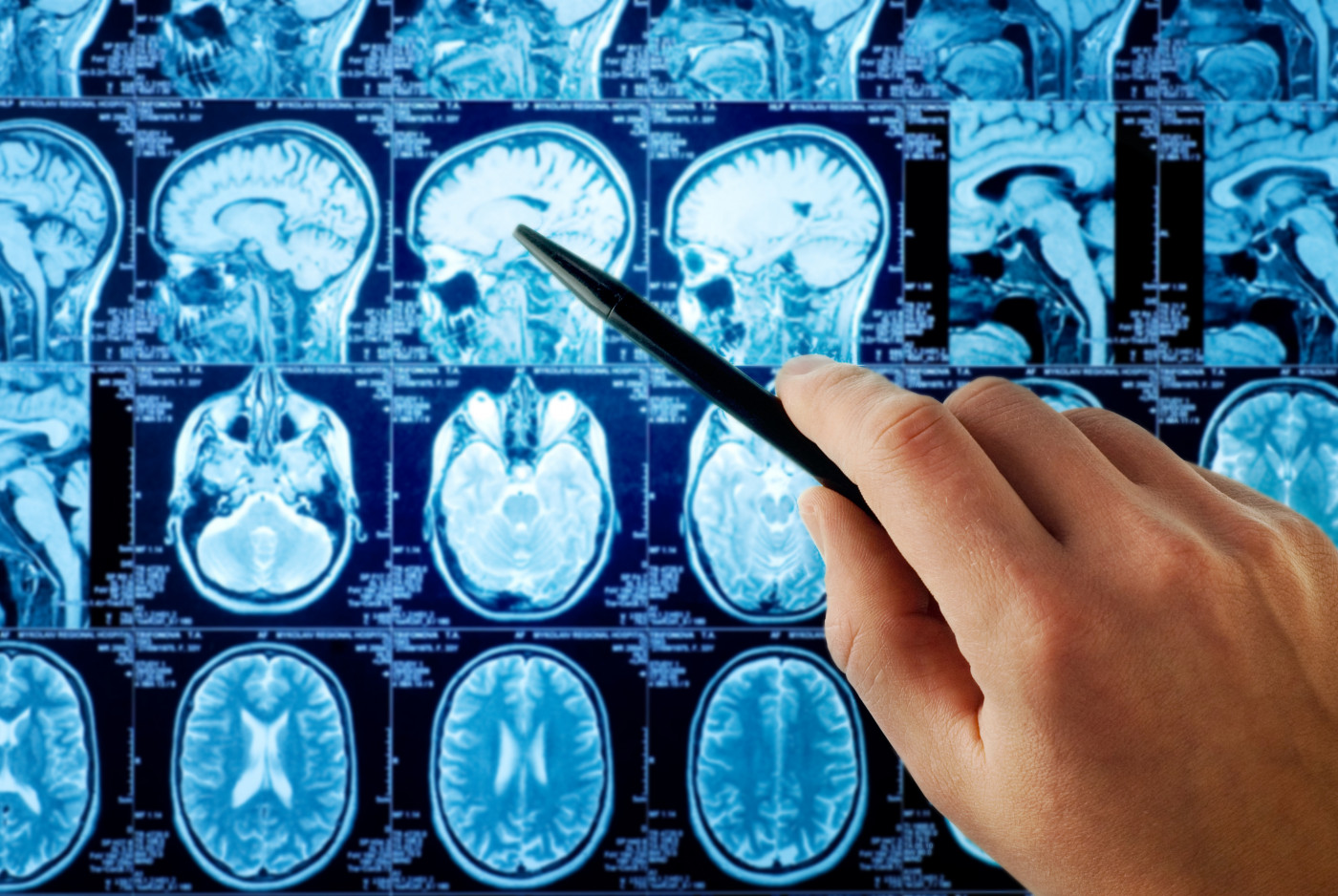
Researchers will compare the cognitive function of those who receive the training with that of controls who do not. One cognitive function yardstick will be changes in patients’ brain structure that show up on magnetic resonance imaging scans.
Another yardstick will be changes in brain function. The team will use both MRI scans and electrophysiology for this measurement. Electrophysiology is a technique that assesses brain activity.
The project grew out of a pilot study in which MS patients and controls completed a computer-based working memory program and a perceptual processing speed training program. The findings suggested that the training led to significant changes in cognitive performance and brain function.
In addition to the effects of the training programs, the research will provide information on nerve-cell networks involved in working memory.
“The study will be the first to examine separately the effects of working memory and processing speed training in adult MS patients,” Dr. Janet L. Shucard, the study’s principal investigator, said in a press release. It will also be “the only study to date to examine the effects of these training paradigms on cognitive performance and on a range of functional and structural neuroimaging measures simultaneously.”
“The strengthening of these cognitive abilities may help to prevent or delay the impact that cognitive deficits have on quality of life, vocational status, and disease-related outcomes,” Shucard added.
Researchers said the second project will be a three-year, $580,000 study on the potential of blocking enzymes called sulfatases to repair the myelin coating that is damaged in MS. The title of the project is “Targeting Extracellular Sulfatases to Accelerate Oligodendrocyte Progenitor-Based Myelin Repair and Regeneration.”
The specific focus of the study will be whether blocking sulfatases can increase oligodendrocyte precursor cells’ ability to mature and start repairing myelin. These cells develop into myelin-producing cells known as oligodendrocytes.
Researchers said the work could lead to new kinds of therapies for reversing MS.
“Importantly, OPCs [oligodendrocyte precursor cells] can generate new oligodendrocytes, restoring lost myelin and promoting functional regeneration,” said Dr. Fraser J. Sim, the study’s principal investigator. “OPCs represent a promising untapped source of stem/progenitors [stem cells and progenitor cells] that when properly stimulated could lead to significant regeneration in MS and other diseases.”
Damaged oligodendrocytes lead to the severe and progressive disability seen in MS. The disease also prevents oligodendrocyte precursor cells from regenerating myelin.
A key part of the project will be studying the role that a biological process called heparin sulfate proteoglycan sulfation plays in MS.
The scientists believe that blocking sulfatases may not only stimulate myelin repair, but also make cells resistant to the MS environment that inhibits repair.
“Sulfation is a biochemical modification that alters how the tissue environment signals to OPCs,” Sim said. “As such, it is in a unique position to alter the chemical communication of OPCs with the inhibitory MS environment.”
This could improve transplanted human cells’ ability to repair the brains of MS patients, he said. “This is important as future transplantation therapies will need to overcome the same inhibitory environment that prevents spontaneous repair.”


