Signaling molecules impair growth of myelin-making brain cells
Pro-inflammatory molecules cause problems, cell study finds
Written by |

Pro-inflammatory signaling molecules that have been implicated in multiple sclerosis (MS) cause problems with the growth and development of myelin-making cells in the brain, according to a study done in cell models.
The findings may have implications for treating MS, as promoting the growth of myelin-making cells could be a strategy for therapeutic approaches, the researchers said.
The study, “Pro-Inflammatory Molecules Implicated in Multiple Sclerosis Divert the Development of Human Oligodendrocyte Lineage Cells,” was published in Neurology Neuroimmunology and Neuroinflammation.
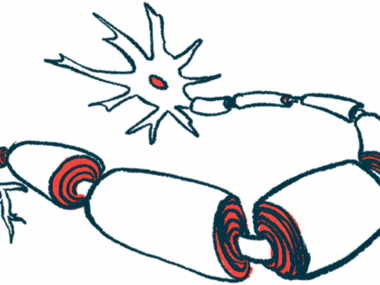
Myelin is a fatty substance that wraps around nerve fibers and helps them to send electrical signals, working like rubber insulation around a metal wire. In MS, inflammation in the brain and spinal cord causes damage to myelin, which leads to problems with neurological signaling that ultimately give rise to disease symptoms.
In the brain, myelin is made mainly by specialized cells called oligodendrocytes. When myelin is damaged, oligodendrocytes can normally spring into action to make new myelin and fix the damage. In MS, the myelin-repairing activity of these cells is impaired. The biological mechanisms that make oligodendrocytes dysfunctional in MS are not fully understood.
Examining signaling molecules
A team led by scientists in Canada conducted a series of experiments to see how certain inflammatory signaling molecules affect the growth of oligodendrocyte precursor cells (OPCs), immature cells that are able to grow into myelin-making oligodendrocytes.
The researchers investigated the effects of tumor necrosis factor-alpha (TNF-alpha) and interferon gamma, both of which are pro-inflammatory signaling molecules that have been shown to play a role in MS-driving inflammation.
“These [inflammatory signaling molecules], among others, are found to be increased in the spinal fluid and peripheral blood of people with MS,” the scientists wrote.
The researchers found that these two inflammatory signaling molecules are not cytotoxic to OPCs. In other words, they don’t kill the immature cells. But exposure to either of the two inflammatory molecules caused OPCs to be less efficient at growing into mature, myelin-making oligodendrocytes.
The researchers noted that OPCs exposed to TNF-alpha tend to take on features of astrocytes, a distinct type of brain cell that helps support nerve function but is not equipped to efficiently make and repair myelin.
“Rather than differentiating into [myelin-making oligodendrocyes], OPCs may instead give rise to astrocytes, contributing to the failure of proper myelin repair,” they wrote.
Though the main experiments were done using cell models, the researchers found astrocyte-like OPCs in damaged brain tissue from MS patients, implying that this mechanism may also occur in people with the disease.
“The identification of this OPC population with an astrocytic gene signature localized within human MS brain lesions may prove a novel mechanism preventing adequate remyelination in an inflammatory context,” the scientists wrote.
The findings point to “a potential therapeutic avenue—strategies aimed at promoting OPC differentiation along the [oligodendrocye] lineage while inhibiting astrocytic conversion could enhance remyelination and mitigate disease progression,” the team concluded.