Stem cell transplant may slow RRMS disease progression: Study
aHSCT linked to reductions in progressive MS biomarkers
Written by |
Autologous hematopoietic stem cell transplant (aHSCT) could slow disease progression in people with relapsing-remitting multiple sclerosis (RRMS), according to a study tracking MS patients in Sweden.
The procedure was associated with sustained reductions in biomarkers linked to progressive MS.
The results also showed that a significant portion of patients (33%) had active disease before the transplant. None of those with available data showed active disease at the one-year follow-up, and only a small fraction showed disease activity two years after aHSCT (3.1%). This low level of disease activity was maintained at the five-year follow-up.
“These exploratory findings suggest that aHSCT may not only induce long-term remission in RRMS but also potentially influence mechanisms related to disease progression,” the researchers wrote.
The study, “Biomarkers of progressive multiple sclerosis decrease following autologous hematopoietic stem cell transplantation,” was published in the Journal of Neuroinflammation.
Resetting the immune system
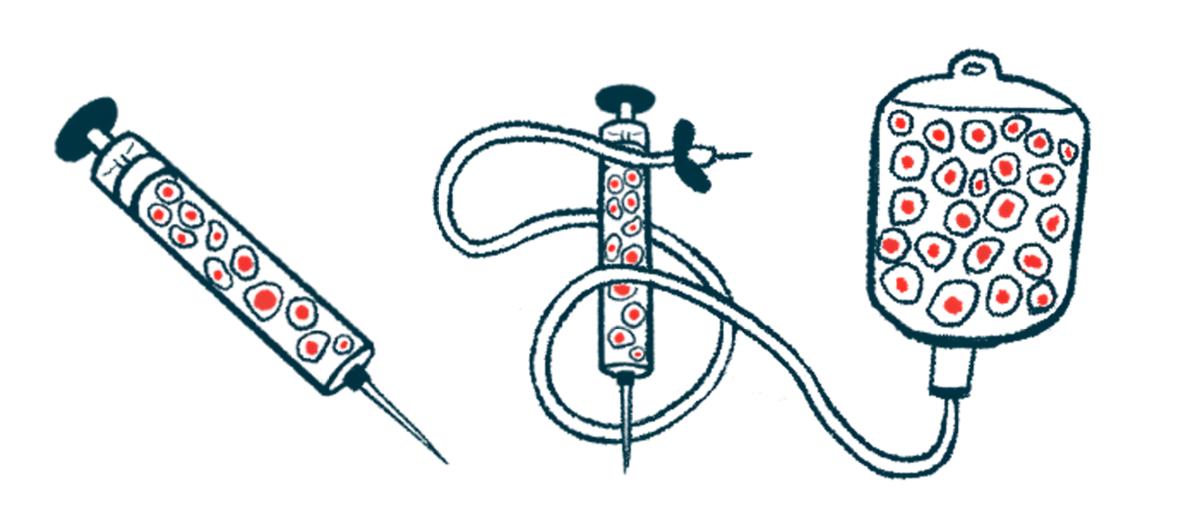
Autologous hematopoietic stem cell transplantation is aimed at resetting a person’s immune system to reduce the excessive inflammation that drives MS. The process begins with collecting hematopoietic stem cells — precursors to most immune cells — from a patient’s bone marrow or blood. Next, chemotherapy eliminates the malfunctioning immune cells. Finally, the stored stem cells are infused back into the patient to rebuild a healthy, normally functioning immune system.
This approach has been recognized as a viable treatment option for severe disease in people with RRMS, proving effective at achieving no evidence of disease activity, meaning no relapses, no worsening disability, and no new lesions. Evidence also suggests that aHSCT might delay or prevent the transition from RRMS to secondary progressive MS (SPMS), a type of MS characterized by gradual neurological decline and disability progression.
In the study, researchers at Uppsala University Hospital in Sweden analyzed whether biomarkers of progressive MS — galectin-9 (Gal-9), GDF-15, and YKL-40 — were affected by aHSCT in people with RRMS. Gal-9 and YKL-40 are associated with acute and chronic inflammatory processes underlying MS, while GDF-15 is linked to mitochondrial dysfunction, a critical mechanism contributing to disease progression.
A total of 45 participants with RRMS, most of them women (64.4%), with a median age of 30 and a median disease duration of 4.3 years, were included. Most participants (88.9%) had been previously treated with disease-modifying treatments (DMTs), and 35 of them were receiving these treatments at the beginning of the study (baseline).
Biomarkers were measured in samples of the cerebrospinal fluid (CSF), the fluid that surrounds the brain and spinal cord. Samples were collected about one day before the mobilization of stem cells, then again 40 days before the cells’ reinfusion, and one, two, and five years after the transplant. Samples from 32 healthy controls were collected once for comparison.
At the beginning of the study, participants with MS had higher levels of progressive MS biomarkers than healthy controls, including Gal-9 (448 vs. 259 picograms per milliliter, pg/mL), GDF-15 (49 vs. 43 pg/mL), and YKL-40 (102 vs. 41 ng/mL).
One year after the stem cell transplant, patients saw significant decreases in the levels of all three biomarkers. Galectin-9 and YKL-40 levels were even lower after two years and remained stable throughout the five-year follow-up, while GDF-15 levels stabilized after the first year.
The levels of these biomarkers were not associated with disease activity, defined as a clinical relapse or active lesions in an MRI scan, either at baseline or during follow-up. They were also not generally related to baseline treatments, except for GDF-15 levels that were significantly lower in participants who were receiving a second line of treatment than in those on a first therapeutic regimen.
Overall, four patients experienced a clinical relapse after the transplant, of whom two also had new inflammatory MRI lesions, after the two-year follow-up. These patients started rituximab. Despite treatment, one had a clinical relapse without new lesions just before the five-year follow-up. In both patients, YKL-40 levels rose before each relapse, whereas Gal-9 and GDF-15 remained unaffected.
“This study provides evidence that aHSCT in RRMS patients leads to a significant and sustained reduction in CSF biomarkers associated with progressive MS,” the researchers wrote, supporting the idea that aHSCT treatment for RRMS could delay or prevent the progression to SPMS. Larger studies are needed to confirm the findings “and better clarify the long-term impact of aHSCT on disease progression and the predictive value of these biomarkers,” they added.



