Measuring Blood Clotting Factor Could Pinpoint RRMS Patients at Risk for Heart Disease
Written by |
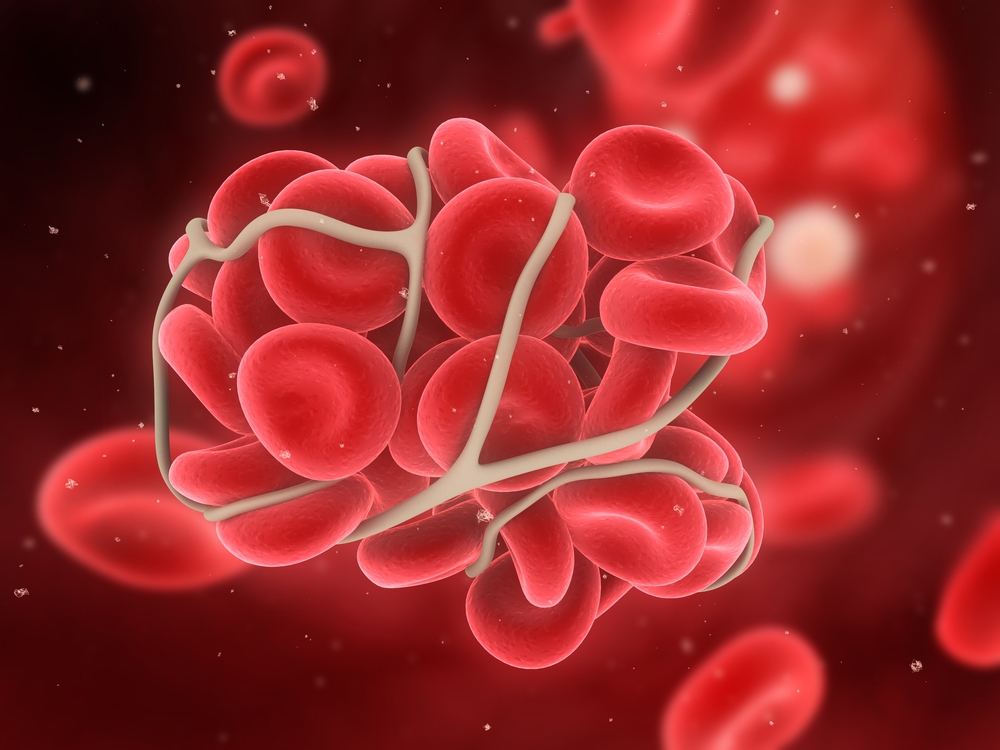
Thrombin, a blood clotting factor, may be involved in the inflammatory processes of multiple sclerosis patients, particularly those with relapsing-remitting form of the disease (RRMS), a study found. Higher levels of thrombin may also explain the increased risk of cardiovascular disease linked to MS.
By measuring thrombin levels, it may be possible to identify MS patients at high risk — potentially preventing heart disease or blood clots before they occur, the research team at Ireland’s University College Dublin argued.
The findings, published in the Multiple Sclerosis Journal — Experimental, Translational and Clinical, also highlight the differences in disease mechanisms between RRMS and primary progressive MS (PPMS).
Thrombin is a well-known component of the blood clotting machinery. But researchers know that the factor is more prevalent in the blood of patients with various inflammatory diseases.
MS patients are more prone to developing cardiovascular disease than the general population. And despite the fact that MS is an inflammatory condition, the link to thrombin has not been explored in MS.
For their study, “Thrombin generation correlates with disease duration in multiple sclerosis (MS): Novel insights into the MS-associated prothrombotic state,” scientists recruited 15 RRMS patients and 15 with PPMS, as well as 19 healthy controls.
At the time of the study, patients had no disease activity and had not been taking disease-modifying medications for six months prior. They were also not allowed to take drugs that interfere with blood coagulation.
Results showed that blood clotting rates were significantly faster in RRMS patients than in people with PPMS and healthy controls. Thrombin was generated at much faster rates in RRMS. Measures in PPMS resembled more those of healthy controls than those of RRMS patients.
Interestingly, the two patient groups differed in how thrombin generation appeared to develop over time.
In PPMS, thrombin generation was highest early after an MS diagnosis, steadily dropping later on. In RRMS, researchers observed the opposite. These patients had low thrombin generation rates soon after diagnosis, while patients with longer disease duration had quicker rates.
Researchers found no links between thrombin generation and disability levels.
The team believes the difference may mirror differences in the inflammatory component of RRMS and PPMS. Researchers think the development of brain and spinal cord lesions in PPMS is less dependent on inflammation than in RRMS.
Thrombin is likely not the only factor influencing the increased risk of blood clotting and heart disease in MS. Some studies also indicate that other components of the clotting machinery are elevated in MS.
While the study was small, researchers said it has a direct implication for MS patients. Keeping track of blood clotting processes may help physicians identify patients at risk of cardiovascular disease — and offering them support and treatment at an early stage.


