Myelin defects seen before lesions, inflammatory activity in MS: Study
Disorganized myelin composition may make brain regions more easily damaged
Written by |

A detailed examination of nerve tissue isolated from multiple sclerosis (MS) patients showed changes to the myelin sheath before the appearance of substantial inflammatory activity and lesions, a study reported.
In MS patients, normal-appearing brain regions showed a less compact, detached, and disorganized myelin composition that may make these regions more susceptible to damage and the formation of lesions.
“We haven’t been able to look at human tissue in such detail before,” Aletta van den Bosch, lead author and a PhD candidate at the Royal Netherlands Academy for Arts and Sciences, in the Netherlands, said in a press release. “This is the first glimpse into what happens at the ultrastructural level in people with MS and what exactly leads to the lesions.”
“It would be great if we could find something to prevent myelin detachment,” van den Bosch said. “While this will not prevent the damage of the lesions that are already there, it might prevent the development of new lesions. This would provide a whole new target for MS treatment.”
The “Ultrastructural Axon–Myelin Unit Alterations in Multiple Sclerosis Correlate with Inflammation” study was published in the Annals of Neurology.
Myelin sheath key to nerve cells functioning
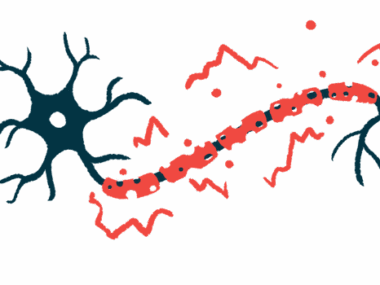
White matter refers to regions of the brain and spinal cord that are mainly made of nerve fibers, or axons. The regions get their name because nerve fibers are surrounded by myelin, a fatty sheath that is whitish in color. The myelin sheath is key for the function of nerve cells, protecting axons and enabling the rapid transmission of electrical signals along axons.
MS is a disease characterized by immune-mediated damage to the myelin sheath and nerve fibers that first appear as lesions arising in white matter regions, which are surrounded by substantial inflammatory activity.
To investigate whether changes in myelin and nerve fibers occur before the appearance of inflammation, researchers examined post-mortem tissue of MS patients and unaffected controls donated to the Dutch Brain Bank. They focused particularly on the optic nerve, which relays information from the eye to the brain, and used an electron microscope to take detailed pictures of white matter regions without obvious lesions.
“To be able to study myelin properly, we looked at the optic nerve. In this area, all nerve fibers and their myelin follow the same direction very nicely, so that we can visualize the myelin well,” van den Bosch said.
Consistent with previous findings, the team confirmed the activation of microglia, the brain’s resident immune cells, and immune T-cells, in normal-appearing white matter (NAWM) from MS patients, compared with control tissue.
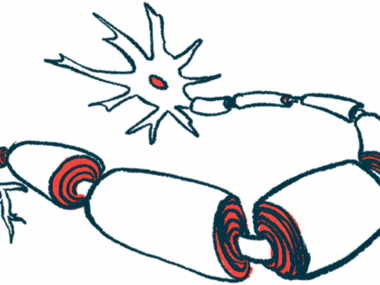
Disorganization of the nodes of Ranvier noted
Microscopic analyses also revealed MS-related disorganization of the nodes of Ranvier, which are gaps in the myelin sheath along myelinated axons. In normal circumstances, electric signals in nerve cells jump from one node to the next, allowing cells to transmit signals 100 times faster.
In MS samples, the length of the node was similar to controls. However, the paranode region, adjacent to the node, and the juxtaparanodal region, next to the paranode, were both elongated and abnormally overlapped in MS tissue.
Measurements made by electron microscopy showed a significantly lower g-ratio in MS samples compared to controls. Defined as the ratio of the inner-to-outer diameter of a myelinated axon, a lower g-ratio in MS tissue reflected a loss of axonal function and integrity. A lower density of myelin also was detected in MS samples.
“There are ultrastructural myelin alterations in MS, as the myelin is less compact in MS NAWM compared to control WM [white matter],” the researchers wrote.
“In MS, myelin was found to be less tightly wrapped around the nerve-fiber,” van den Bosch said. “This means that the fiber is not properly insulated which has major consequences: the signal can’t be transmitted as fast as it used to be. We saw that where myelin was less attached to the fiber, there was a disruption of the nodes of Ranvier combined with increased levels of T-cells and activated microglia.”
More energy-generating mitochondria present
Compared with healthy WM, MS nerve fibers contained more energy-generating mitochondria, implying “a higher axonal energy demand or a stagnated mitochondrial transport in MS NAWM compared to control WM,” the researchers noted.
“There were more mitochondria,” van den Bosch said. “Mitochondria are the energy factories of the cell, so this phenomenon may indicate that more energy is needed for signal movement and maintenance of the fibers.”
However, excess mitochondria can increase the risk of oxidative stress, an accumulation of tissue-damaging oxygen free radicals generated as products of the cells’ metabolism.
“Although mitochondria are generally good for energy production, they also produce many by-products, such as oxygen radicals,” van den Bosch added. “We suspect this to be an amplifying factor for myelin breakdown: the myelin is already in a bad state, more mitochondria develop to provide more energy, which then makes conditions even worse.”
Lastly, myelin defects, including a lower myelin density and higher mitochondria numbers, correlated with signs of inflammation in MS tissue, such as the number of activated microglia or T-cells. Longer paranodes and juxtaparanodes, and the percentage overlap between these regions, also correlated with immune cell activation.
However, because it remained unclear if inflammation was causing the alterations or if the inverse was happening, “future research is necessary to elucidate any causalities,” the team wrote.
“Our data show ultrastructural changes in the NAWM of MS at the levels of the myelin and axon,” the researchers concluded. “Moreover, the changes correlated with chronic inflammation throughout the [brain and spinal cord]. These changes may contribute to further MS progression.”
According to van den Bosch, “the next step is to see if we can prevent the myelin from winding so loosely around nerve endings. First, we want to experiment in culture dishes to see if we can make the wrapping of myelin stronger. Subsequently, we will have [to] perform tests in laboratory animals, and eventually we will be able to take the step to humans.”