New Clinical Trial Data on Experimental MS Therapeutic Vaccine, Xemys, Released
Written by |
PJSC Pharmsynthez, a pharmaceutical company based in Russia, recently announced completed follow-up findings and data analysis from a Phase 2a proof-of-concept clinical trial of its novel therapeutic vaccine Xemys for the treatment of multiple sclerosis (MS). Xemys utilizes Xenetic Biosciences patented ImuXen technology.
In the open-label, dose-escalating trial, 20 patients with a diagnosis of relapsing-remitting multiple sclerosis (RRMS) or secondary progressive multiple sclerosis (SPMS) were treated weekly with ascending doses of Xemys for a period of six weeks. The maximum dose was 2.675 mg.
Enrolled patients had meaningful disease activity despite treatment with glatiramer acetate or interferon-beta (IFN-b), with 34 disease relapses in the year prior to study enrollment.
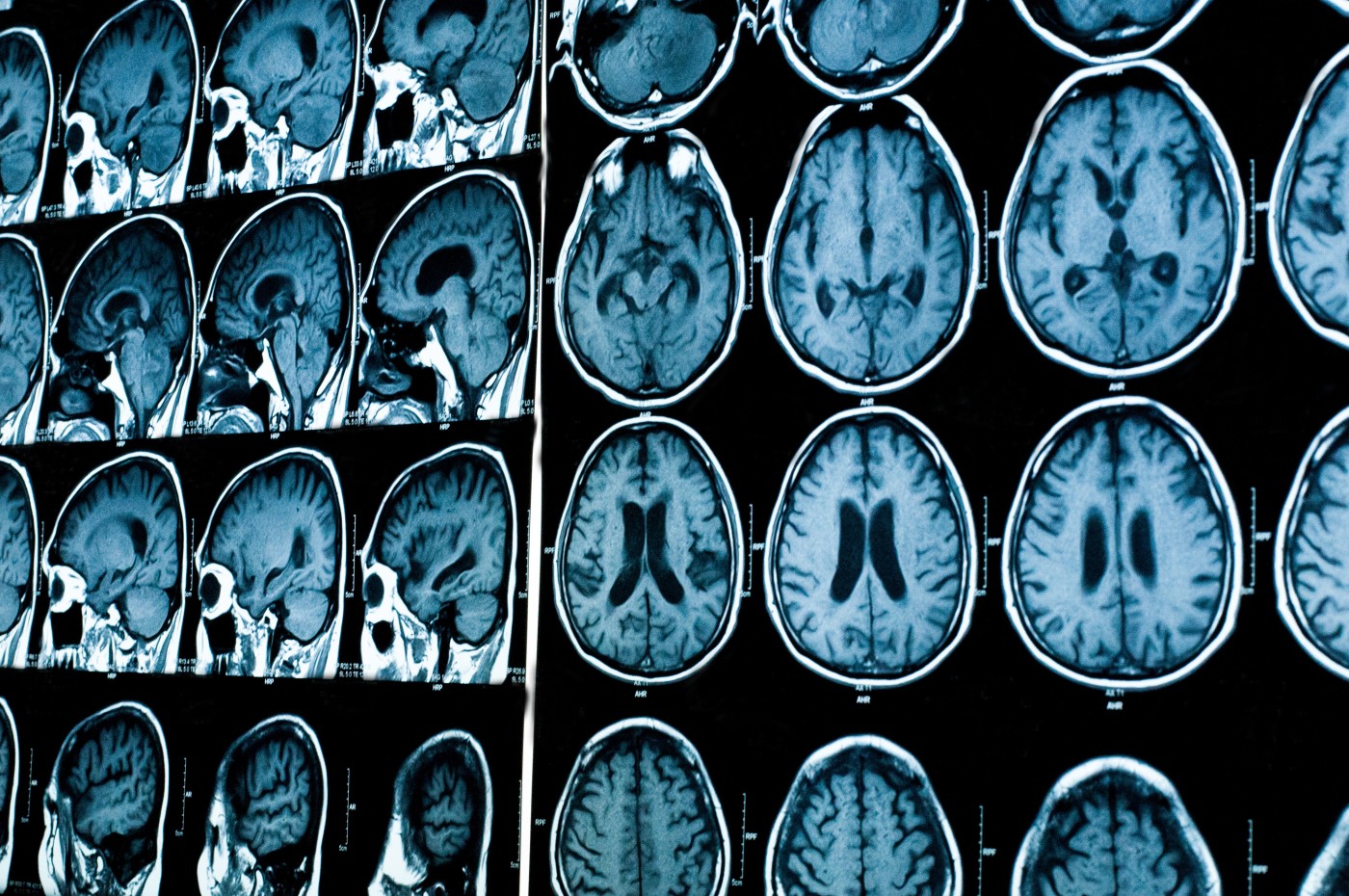
Before the first injection of Xemys, during the treatment period, and after 17 weeks of follow-up, all patients were clinically assessed through magnetic resonance imaging (MRI), expanded disability scale score (EDSS), and levels of serum cytokines.
Data showed that the EDSS scores, and the amount of T2 lesions and new gadolinium-enhancing lesions based on MRI, were unchanged at the end of the trial, the company said in a press release. Decreases were observed in the levels of the serum cytokines MCP-1, MIP-1, and IL-7. The levels of TNF (or tumor necrosis factor, found in active MS lesions) increased during the treatment period.
Subcutaneous injections of Xemys were found to be well-tolerated in patients who had previously not achieved a sustained control of their disease with glatiramer acetate or IFN-b. Patients experienced mild or moderate adverse events related to treatment with Xemys, and these were found to occur mostly with submaximal and maximal dosing. No concomitant medication was required to manage the adverse events.
Twenty weeks after study enrollment, seven patients (37%) had no evidence of disease activity as measured by NEDA (No Evidence of Disease) scores, and 16 patients (85%) were free of relapse. Only three patients experienced relapses during the trial. There were statistically meaningful increases in the number of gadolinium-enhancing lesions, but these were only evident in patients who had experienced disease relapse.
RRMS — the most common disease course — is characterized by clearly defined periods of relapse or exacerbation attacks and new or increasing neurologic symptoms, followed by periods of partial or complete recovery (remissions). During remissions, all symptoms may disappear, or some symptoms may continue and become permanent, but there is no apparent disease progression during the periods of remission. Approximately 85 percent of people with MS are initially diagnosed with RRMS.
SPMS follows RRMS. In SPMS, disability gradually increases over time, with or without evidence of disease activity (relapses or changes on MRI).


