Low Neurite Density in Spinal Cord Linked to Greater Physical Disability in RRMS Patients
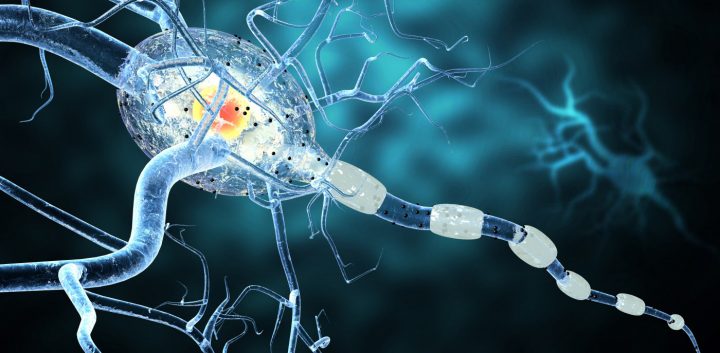
Photo by Shutterstock
People with relapsing-remitting multiple sclerosis (RRMS) have poorer neurite density — a measure that relates to the amount of nerve cell projections, including axons and dendrites involved in nerve-to-nerve communication — in the brain and spinal cord than do those without this disease, a study shows.
This measure, especially in the spinal cord, correlates with physical disability, its researchers report.
Their study, “Reduced neurite density in the brain and cervical spinal cord in relapsing-remitting multiple sclerosis: A NODDI study,” was published in the Multiple Sclerosis Journal.
Neuronal degeneration is a significant component of disease progression in MS. However, exactly how specific alterations in nerve cells of the brain and spinal cord relate to physical and cognitive disability is not clear.
Quantitative magnetic resonance imaging (MRI) studies of the central nervous system in MS patients could help in understanding this relationship, but the time required to build the series of scans that might relate neurodegeneration to disability weighs against this approach.
Neurite orientation dispersion and density imaging (NODDI) is a MRI technique that allows scientists to evaluate, specifically and accurately, the structure of brain tissue. It provides values that relate to neurite density and orientation, which indirectly indicate neurodegeneration.
Researchers at University College London assessed how changes in neurite density and orientation, as determined by NODDI, related to physical and cognitive disability in RRMS patients.
Using it, they assessed the brain and cervical spinal cord — the spine’s top portion, corresponding to neck vertebrae — of 28 RRMS patients, between 18 and 65, and compared the results to those of 20 healthy controls of similar age and gender.
Results showed that RRMS patients had a lower neurite density in the brain and cervical spinal cord than controls, even in regions with no apparent lesions.
Patients who had a lower neurite density in the spinal cord also had greater physical disability.
“This suggests that a reduced neurite density, which is a known component of neurodegeneration, may contribute to neurological impairment in MS,” the researchers wrote.
No significant correlation was seen between low neurite density in the brain and increased disability.
Measures of cognitive disability also did not correlate with abnormal NODDI parameters. “Further studies analyzing NODDI in specific cortical regions, and linking them with the corresponding cognitive domains are needed,” the reseatchers wrote.
These results suggest that “neurite integrity loss, which is a crucial element of neurodegeneration, occurs in both the brain and spinal cord in MS, but mainly when affecting the cervical cord, it may contribute to physical disability,” the team concluded.
NODDI protocols are currently not available in clinical practice. But the researchers suggested that clinical trials could use spinal cord NODDI results as a marker of disability when assessing the efficacy of neuroprotective treatments.