New Mechanism Boosting Myelin Regeneration May Ease MS Symptoms, Mouse Study Shows
Written by |
Blocking a protein called PAR1 may enhance the regeneration of myelin, the protective fatty layer that covers nerve fibers and is damaged in multiple sclerosis (MS), a mouse study shows.
Therapeutic targeting of PAR1 may promote remyelination and delay MS progression, according to the study, “Blocking the Thrombin Receptor Promotes Repair of Demyelinated Lesions in the Adult Brain,” published in the Journal of Neuroscience.
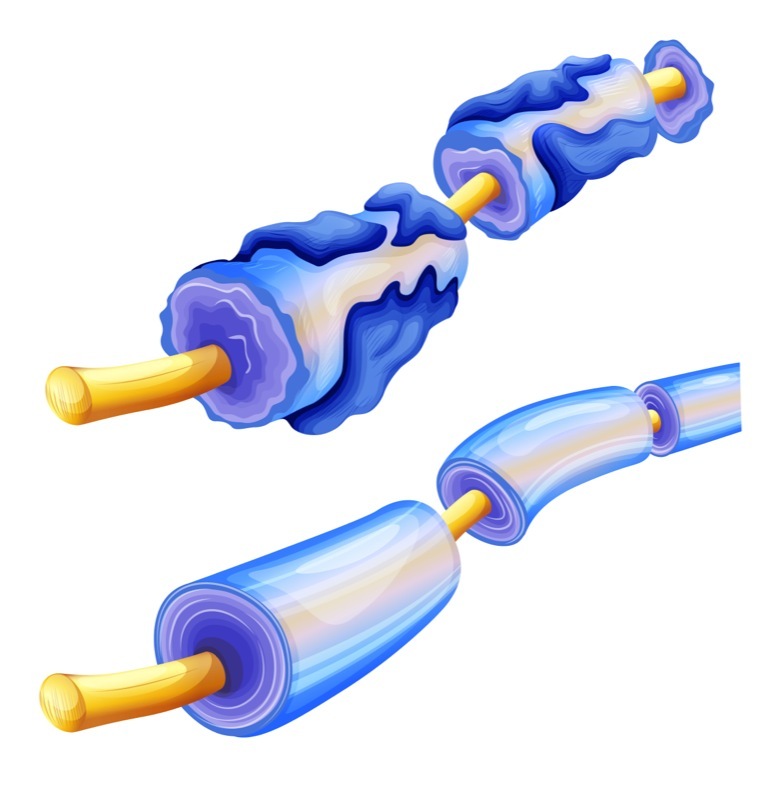
Myelin, which coats nerve fibers — or axons — provides protection and support to electric signal transmission between neurons, working as a wire insulator. In demyelinating diseases such as MS, myelin is damaged and electrical signals take longer to be transmitted, resulting in a loss of sensory and motor function. Losing this protection also leaves nerves more prone to degeneration.
Previous studies have shown that oligodendrocyte progenitor cells (OPCs) can be found in some MS lesions. OPCs have the potential to transform, or differentiate, into mature oligodendrocytes, which are cells that produce myelin in the central nervous system (brain and spinal cord). However, despite the presence of these progenitor cells in MS lesions, remyelination is incomplete or absent.
“These oligodendroglia fail to differentiate into mature myelin regenerating cells for reasons that remain poorly understood,” lead author Isobel A. Scarisbrick, PhD, of the Mayo Clinic School of Biomedical Sciences Rochester, said in a press release.
In a previous study, researchers discovered that high levels of a class of proteins called serine proteases suppressed the differentiation of oligodendrocytes, affecting myelination. In particular, thrombin and its receptor protein, protease activated receptor 1 (PAR1), were found to be key players in this process.
The team investigated whether PAR1 could be involved in myelin regeneration, using two mouse models of demyelination: one generated by injecting lysolecithin into the spinal cord to induce local loss of myelin, and the other by administering oligotoxin cuprizone to the animals’ diet to induce global demyelination of the corpus callosum, which is a large group of nerve fibers that connect both sides of the brain.
In the first model, genetic deletion of PAR1 led to a significant increase in remyelination. Fourteen days after the lysolecithin injection, mice without PAR1 had a 1.8 times increase in the number of remyelinated axons, and a 1.4 times increase after 28 days relative to control mice. The activity of oligodendrocyte specific genes was also increased when PAR1 was removed.
In the second model, researchers observed that mice without PAR1 had improved myelin regeneration at three and six weeks after the cuprizone diet. This improvement was accompanied by increases in the number of mature oligodendrocytes.
To test if myelin regeneration had an actual effect on the neuron’s function, in particular motor coordination and strength, researchers used the accelerated rotarod paradigm, a test in which mice are placed on top of a circular rod turning at increasing speed.
Mice without PAR1 were able to maintain their balance at a higher angular speed than controls, suggesting “that PAR1 loss of function during the period of demyelination has the potential to preserve neurological function,” the researchers said.
Deleting PAR1 also led to less neuroinflammation caused by astrocytes and microglia cells, a hallmark of MS, the researchers said. In fact, they observed that astrocytes — specialized cells that protect and support neurons — changed their behavior to a pro-repair response.
“Our research identifies PAR1 as a molecular switch of myelin regeneration,” Scarisbrick said. “In this study, we demonstrate that blocking the function of the PAR1, also referred to as the thrombin receptor, promotes myelin regeneration in two unique experimental models of demyelinating disease.”
At the molecular level, PAR1 loss in astrocytes increased the expression of brain-derived neurotropic factor and insulin-like growth factor 1, two growth factors that promote neuron proliferation and their proper function, working as pro-myelinating factors.
These findings indicate that blocking PAR1 helps to increase oligodendrocyte numbers and acts on reactivating astrocytes’ repair response.
“Myelin regeneration holds tremendous potential to improve function,” Scarisbrick said. “We showed when we block the PAR1 receptor, neurological healing is much better and happens more quickly. In many cases, the nervous system does have a good capacity for innate repair.”
“This sets the stage for development of new clinically relevant myelin regeneration strategies,” she said.
Researchers then tested vorapaxar, a small-molecule inhibitor of PAR1, in OPCs derived from healthy mice or those without PAR1. Treatment with vorapaxar induced the differentiation of OPCs into oligodendrocytes, similar to the genetic strategy used in the previous mouse models.
Treating astrocytes alone with vorapaxar and co-culturing them with OPCs led to an increasing differentiation of these cells into oligodendrocytes, demonstrating that blocking PAR1 in astrocytes activates signaling pathway(s) that promote myelin regeneration.
Zontivity (vorapaxar) is a PAR1 antagonist that prevents blood clot formation, and was approved in 2014 by the U.S. Food and Drug Administration to treat patients with a history of myocardial infarction (heart attack) and peripheral arterial disease.
Further research is needed before testing vorapaxar in MS patients, the researchers said.
“It is important to say that we have not and are not advocating that patients take this inhibitor at this time,” Scarisbrick said. “We have not used the drug in animals yet, and it is not ready to put in patients for the purpose of myelin repair. Using cell culture systems, we are showing that this has the potential to improve myelin regeneration.”


