Mechanism Controlling Remyelination May Have MS Therapy Implications, Study Finds
Written by |
Chemical modification of the protein eukaryotic elongation factor 1A1 (eEF1A1) regulates remyelination, a new study suggests, indicating that the processes regulating this protein may provide useful therapeutic targets for multiple sclerosis (MS).
The study, “EEF1A1 deacetylation enables transcriptional activation of remyelination,” was published in Nature Communications.
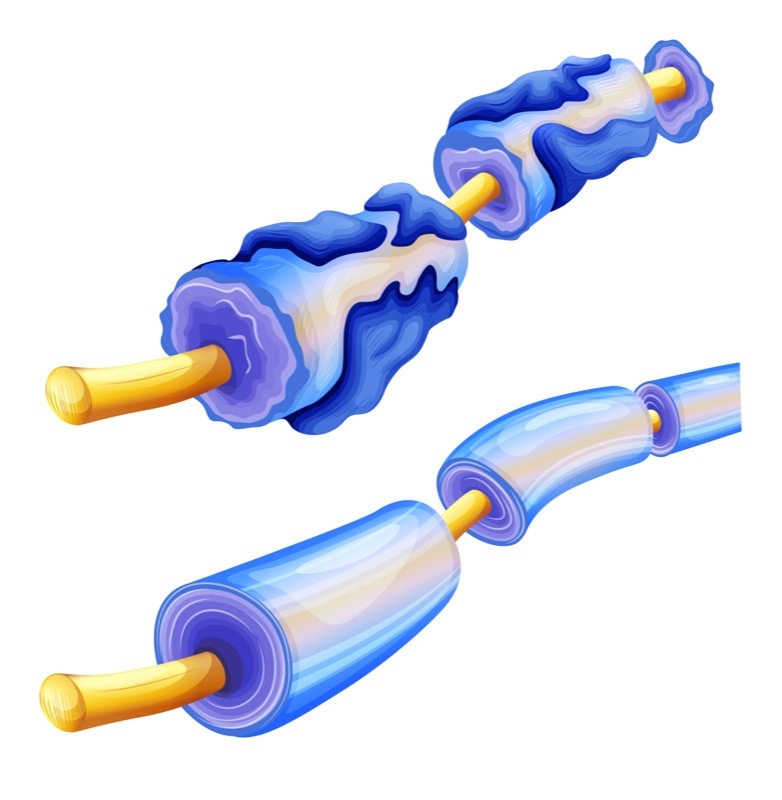
Myelin is a “sheath” of protein and fat molecules that wraps around neurons and is critical for proper neuronal function. MS and some other neurological conditions are characterized by a loss of myelin. Restoring lost myelin — termed remyelination — is a goal of MS research.
The nervous system can be broadly divided into two parts: the central nervous system (CNS), consisting of the brain and spinal cord, and the peripheral nervous system (PNS), which encompasses everything else. When neuronal damage occurs, remyelination can occur in the PNS, but in the CNS it is more limited and less efficient for reasons that are not fully understood.
“In order to promote the restoration of myelin, we need to understand the process that controls the mechanism,” Claire Jacob, co-author of the study and professor at Johannes Gutenberg University Mainz in Germany, said in a press release.
Previous research implicated the protein SOX10 in remyelination, in both the PNS and the CNS.
SOX10 is a transcription factor — a protein responsible for controlling gene expression (the extent to which different genes are turned “off” or “on”). When SOX10 is active, it promotes the activity of genes linked to remyelination. However, the factors that regulate SOX10 itself have not been fully elucidated.
Previous research showed that two related proteins, HDAC1 and HDAC2, are necessary for SOX10 function. These proteins regulate acetylation — a type of chemical modification involving the addition of an acetyl group, which can regulate protein function.
In the new study, researchers investigated how remyelination occurs in the PNS and CNS using mice models of nerve damage wherein HDAC1 and HDAC2 were inhibited.
“First, we wanted to understand the process that blocks remyelination. We subsequently studied how to counteract this blocking effect,” Jacob said.
Results showed that HDAC1 and HDAC2 regulate the acetylation of eEF1A1; specifically, HDAC1/2 act by removing the acetyl group from eEF1A1.
Further experiments revealed that acetylated eEF1A1 (Ac-eEf1A1) was present in the nucleus (the cellular component that houses DNA) of myelin-producing cells, whereas deacetylated eEf1A1 was not. The team determined that Ac-eEf1A1 in the nucleus was able to interact with SOX10, causing the latter to move out of the nucleus.
In other words, “Ac-eEF1A1 drags Sox10 out of the nucleus,” the researchers wrote.
As a transcription factor, SOX10 is able to enact its pro-remyelination function only when it is in the nucleus. As such, the data suggest that, by removing SOX10 from the nucleus, Ac-eEf1A1 prevents remyelination.
Conversely, since HDAC1/2 remove the acetyl group from Ac-eEf1A1, these data suggest that activating HDAC1/2 could reduce the levels of Ac-eEf1A1 in cells, subsequently increasing the amount of SOX10 in the nucleus and, ultimately, promoting remyelination.
“Once we understood this process, we decided to try to control it by boosting the HDAC2 activity and its synthesis in cells,” Jacob said.
Theophylline is a medication used to treat breathing difficulties in conditions like asthma. Theophylline can have different biological effects depending on its concentration; at low doses, it is known to activate HDAC2. As such, researchers hypothesized that theophylline treatment might promote remyelination.
The team tested theophylline treatment in mouse models of nervous system damage. Results showed that, in both the PNS and the CNS, theophylline treatment increased levels of HDAC2 and Sox10 and improved remyelination. These positive effects were seen in both young and old mice. (Notably, the body’s remyelination ability is known to decrease dramatically with age.)
Notably, additional experiments using drugs to affect other potential targets of theophylline did not have this effect, indicating that the effect was specifically due to theophylline’s activation of HDAC2.
Overall, “a short treatment with theophylline in mice increased HDAC2 expression, decreased Ac-eEF1A1 levels, increased the expression of Sox10 and its target genes and improved remyelination efficiency in both PNS and CNS,” the researchers wrote.
“Of major importance, theophylline also increased the efficiency of CNS remyelination in old mice, thereby suggesting a potential beneficial effect on the remyelination process in aged individuals, where remyelination is strongly impaired,” the team added.
Based on the results, the team suggested that theophylline is “a very promising compound to test in future translational studies to accelerate and promote remyelination after traumatic lesions or in the context of demyelinating disorders” like MS.


