Impact of Gut Microbiota in MS More Complex Than Thought, Study Shows
Written by |
The presence of a particular gut bacterium widely used in probiotics, called Lactobacillus reuteri (L. reuteri), was sufficient to increase disease severity in a mouse model of multiple sclerosis (MS), but only in genetically susceptible animals, a recent study shows.
These findings highlight the complex interactions between gut microbiota and genetic background in driving MS susceptibility. They also may explain the conflicting reports on the anti- or pro-inflammatory roles of specific gut microbiota species.
The researchers say the study results also suggest that therapeutic strategies targeting the gut microbiota in MS — some are already underway — should consider host genetics and the pre-existing gut microbiota.
“Our gut bacteria are part of a complex ecosystem that holds great potential for the prevention, treatment, and/or diagnosis of chronic diseases,” Dimitry Krementsov, PhD, the study’s senior author and an assistant professor in the department of biomedical and health sciences at the University of Vermont, said in a press release.
“However, many scientists have been going at it with a one-size-fits-all approach, and our research suggests that this is unlikely to work,” Krementsov added. “Instead, a more personalized approach is needed.”
The study, “Interactions between host genetics and gut microbiota determine susceptibility to CNS autoimmunity,” was published in the journal Proceedings of the National Academy of Sciences.
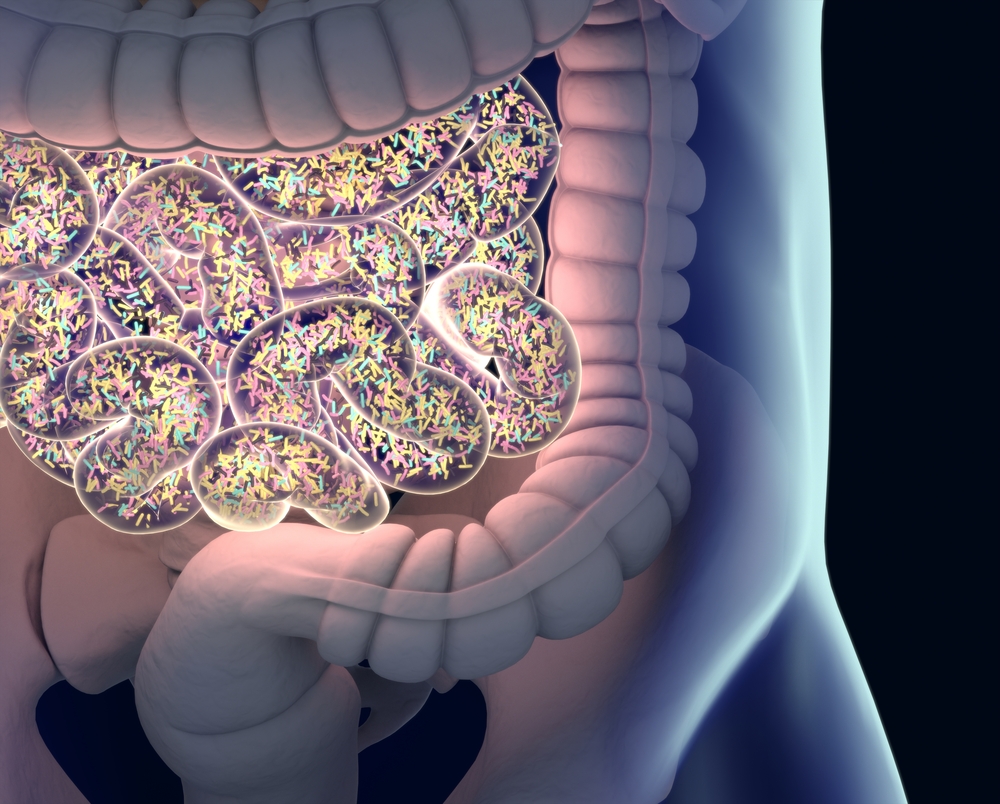
Gut microbiota comprises the vast community of friendly bacteria, fungi, and viruses that colonize the gastrointestinal tract. This community helps to maintain a balanced gut function and protect against disease-causing microorganisms. It also influences the host’s immune system and inflammatory responses.
Increasing evidence supports gut microbiota as an important contributor to MS development or severity, with MS patients showing a gut microbiota imbalance toward pro-inflammatory microbes.
Therefore, manipulation of the gut microbiota — either through antibiotics or probiotics — may potentially promote therapeutic benefits in MS patients. Of note, probiotics, found in yogurt and dietary supplements, are live microorganisms thought to improve gut health.
Considerable efforts are currently focused on the development of such strategies.
“However, the identity of gut microbes associated with disease risk, their mechanisms of action, and the interactions with host genetics remain obscure,” the researchers wrote, noting that the impact of the host’s natural genetic variation “has been largely overlooked.”
Now, researchers at the University of Vermont, along with colleagues in the U.S. and Germany, showed that specific gut bacteria may be “good” or “bad” for MS depending on the host’s genetic background.
The team used two genetically distinct mouse strains known to have different susceptibilities: the experimental autoimmune encephalomyelitis or EAE, an MS-like autoimmunity mouse model, and a genetically diverse mouse model representing 27 unique strains with a mixed genetic background. Of note, a strain is a group of mice in which all are as genetically identical as possible.
Each of these mixed strains — called consomic strains and often used in genetic studies — contained only one particular chromosome from the EAE-resistant strain, with the remaining genome deriving from the EAE-susceptible strain.
With this genetic variability across strains, the researchers were more likely to pinpoint the potential genetic-gut microbiota interactions behind MS susceptibility.
Indeed, this approach highlighted the presence of gut microbiota profiles specific to different genetic backgrounds, confirming an association between genetic and gut microbiome diversity. Gut microbiota composition also was found to predict EAE susceptibility in these mice.
To the researchers’ surprise, gut microbiota manipulation experiments showed that EAE was significantly more severe in germ-free EAE-susceptible mice when their gut was colonized with gut microbiota from EAE-resistant mice than from EAE-susceptible mice.
Further analysis identified L. reuteri as the potential culprit for the observed EAE aggravation in susceptible mice. The introduction of this bacterium was “sufficient to exacerbate EAE … in a genetically susceptible host,” the researchers wrote. L. reuteri is a bacterium present in human and mouse gut and used in probiotics due to its potential beneficial effects.
“These data illustrate L. reuteri’s potential to skew host immune cell repertoires to either pro- or antiinflammatory in a context-dependent fashion, as influenced by window of exposure, host genetics, and the microbiome ecosystem within which it resides,” the team wrote.
“We conclude that genetic predisposition plays a primary role in setting the required ‘minimal baseline’ of MS susceptibility, while the gut microbiota play a secondary role in modulating this susceptibility, possibly tipping the scale above or below a critical threshold for disease initiation or progression,” the researchers wrote.
Regarding the potential benefits of probiotics, the team noted that the study addressed the role of gut microbiota as a risk factor for MS, rather than as a therapeutic probiotic intervention. The researchers also noted that probiotic bacteria are genetically distinct from their naturally occurring counterparts.
Overall, the findings add new layers to the already complex interactions behind MS susceptibility and highlight “the need to consider both host genetics and [pre-existing] gut microbiome composition in probiotic or similar therapeutic strategies, especially given that such efforts are already underway in MS,” the team concluded.


