Omega-3 fatty acid transporter vital for myelin sheath production: Study
Oligodendrocytes fail to mature in mice that lack Mfsd2a protein
Written by |
A protein called Mfsd2a, which transports molecules that contain omega-3 fatty acids, is essential for regulating cells that make the fatty coating on nerve fibers, or myelin sheath, that’s damaged in multiple sclerosis (MS), a study indicates.
In mice lacking Mfsd2a, the cells that make myelin, or oligodendrocytes, fail to mature, leading to a decline in cellular levels of omega-3 fatty acids and a reduction in myelination.
“Our study indicates that [omega-3 molecules] act as factors within the brain to direct oligodendrocyte development, a process that is critical for brain myelination,” David Silver, PhD, the study’s senior author and deputy director of the Cardiovascular & Metabolic Disorders program at Duke-NUS Medical School, Singapore, said in a university press release. “This opens up potential avenues to develop therapies and dietary supplements based on [omega-3] that might help retain myelin in the aging brain — and possibly to treat patients with neurological disorders stemming from reduced myelination.”
The study, “Deficiency in the omega-3 lysolipid transporter Mfsd2a leads to aberrant oligodendrocyte lineage development and hypomyelination,” was published in the Journal of Clinical Investigation.
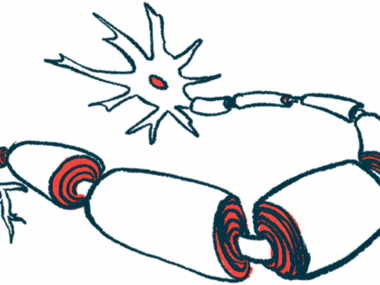
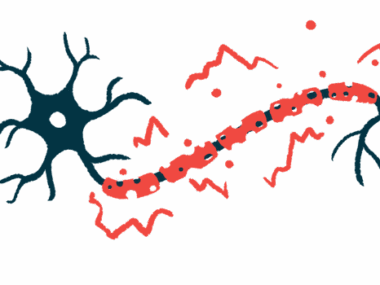
A feature of MS is immune-mediated damage to the myelin sheath, a protective coating composed mostly of fat molecules (lipids) and several specialized proteins. This damage can occur in other neurodegenerative diseases too, such as Alzheimer’s disease, and as part of aging.
“Loss of myelin sheaths occurs during the normal aging process and in neurological diseases, such as multiple sclerosis and Alzheimer’s disease,” said study co-lead Sengottuvel Vetrivel, PhD, a senior research fellow at Duke-NUS. “Developing therapies to improve myelination — the formation of the myelin sheath — in aging and disease is of great importance to ease any difficulties caused by declining myelination.”
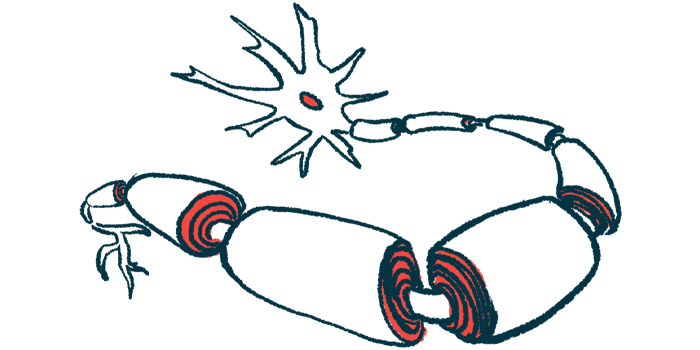
As part of the myelination process, Mfsd2a transports lysophosphatidylcholine (LPC), a lipid that contains an omega-3 fatty acid, into oligodendrocytes. Thus, genetic defects resulting in a Mfsd2a deficiency lead to reduced myelination and cause microcephaly, a congenital disability marked by a smaller than normal head size.
While the mechanisms that link Mfsd2a’s function to brain growth are established, how the LPC transport is critical for myelination is less clear.
To learn more, Vetrivel and Silver, who previously discovered that Mfsd2a is an LPC transporter, deleted the gene that encodes for the protein in mice. These mice showed reduced myelination (hypomyelination) and microcephaly, like human patients do.
Mice without Mfsd2a don’t develop cells that make nerve fibers’ coating
As with previous studies, Mfsd2a production occurred in oligodendrocyte precursor cells (OPCs), which eventually develop into mature, myelin-producing oligodendrocytes.
Deleting Mfsd2a specifically in OPCs showed a marked reduction in three myelin proteins and in myelination as early as eight days after birth. But unlike mice lacking Mfsd2a across all cells, these mice had typical brain sizes and no signs of microcephaly.
“These findings demonstrate that loss of Mfsd2a in OPCs leads to hypomyelination during early postnatal development,” the team wrote.
The researchers then investigated the impact of Mfsd2a deletion on the mouse oligodendrocyte developmental lineage. OPCs, which are derived from neural progenitors, become fully mature myelin-producing cells via several stages of immature cells.
Single-cell analysis of this lineage revealed that deleting Mfsd2a from OPCs didn’t affect the total number of each cell type, but the stage of the oligodendrocyte development instead.
As a result, OPCs without Mfsd2 rapidly transformed into large numbers of immature oligodendrocytes with altered gene regulation in multiple pathways, including lipid metabolism. At the same time, the progression from immature cells into fully mature myelinating oligodendrocytes was suppressed.
Lipid analysis of OPCs and immature cells from mice lacking OPC-specific Mfsd2a showed reduced lipids containing omega-3 fatty acids with an opposing increase in unsaturated fatty acids. Srebp-1, a pathway involved in producing these unsaturated fatty acids, was activated alongside the impaired activity of regulators of oligodendrocyte development.
“Overall, altered lipid composition and associated gene expression [activity] changes correlate with the disruption in the normal progression of oligodendrocyte development, leading to hypomyelination,” wrote the researchers, who noted it was important to determine if supplementing with omega-3 fatty acids could promote remyelination in diseases like MS, and in aging.
“We’re now aiming to conduct preclinical studies to determine if dietary LPC omega-3 can help to re-myelinate damaged axons in the brain,” Silver said. “Our hope is that supplements containing these fats can help to maintain — or even improve — brain myelination and cognitive function during aging.”
Patrick Casey, PhD, senior vice dean for research at Duke-NUS, said Silver has relentlessly investigated the “far-reaching role” of the important lipid transport protein Msdf2a, suggesting avenues may be available to treat both the aging brain as well as other organs where it “plays a role.”