MS lesions grow from center outward, new mapping study shows
Lesions found to start as small core of inflammatory immune cells
Written by |
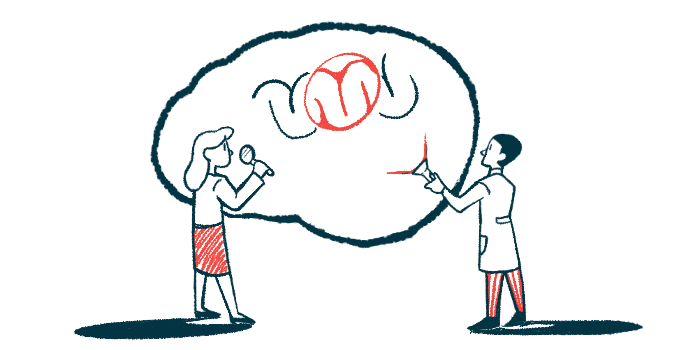
In multiple sclerosis (MS), lesions — areas of abnormal tissue in the nervous system — start as a core of a few inflammatory immune cells, with inflammatory damage then spreading outward from these cells to form a lesion.
That’s according to a new study from Sweden, in which researchers mapped lesions in a mouse model of MS. Titled “Cellular architecture of evolving neuroinflammatory lesions and multiple sclerosis pathology,” the study was published in the journal Cell.
There’s been debate in the MS field as to whether lesions develop centrifugally, meaning from the center out, or centripetally, from an outer ring toward the center. These data suggest the former is more likely.
MS is marked by such lesions, where nervous tissue has become inflamed and damaged, in the brain and spinal cord. But even though lesions are a defining feature of MS, not much is known about how they develop at a cellular level.
That lack of data led a team of scientists to conduct a series of tests using mice with experimental autoimmune encephalomyelitis (EAE), a lab-induced disease used to model MS.
“We wanted to understand which cells are part of the lesions and their dynamics over time,” Petra Kukanja, co-first author of the study and a PhD student at Karolinska Institutet, in Stockholm, said in a press release.
Scientists seek to settle debate over how MS lesions develop
In their study, the researchers examined the cellular evolution of lesions over time using a technique called in situ sequencing. This basically involves measuring the activation of hundreds of genes, cross-referenced against data about where the cells are placed in physical space, to provide a comprehensive map of cell activity and interactions.
By taking samples at multiple points in disease development, the researchers could compare how cell activity changed as EAE progressed.
From these analyses, the team identified several noteworthy findings. For one, in the earliest stages of the disease, inflammatory immune cells first enter the spinal cord before moving to the brain.
Signs of early lesions were seen throughout the spinal cord, but in some parts, the early inflammation was less likely to resolve, so these regions were more likely to develop long-term lesions, the team found.
“Lesions consistently affect certain spinal cord regions and persist throughout the late EAE stage at specific locations,” the scientists wrote.
The team also found that these EAE lesions tend to develop in a centrifugal manner — that is, the lesions start with a few abnormal inflammatory cells, and then inflammation and damage spread outward from those cells, which eventually become the center of the lesion.
Christoffer Mattsson Langseth, co-first author of the study and a PhD student at Stockholm University, described the lesions as being “built up centrifugally in two dimensions, with immune cells in the middle and different types of glial cells around them.”
Glial cells, often simply called glia, are a broad class of brain cells that support neural function. It’s long been known that MS lesions contain abnormal disease-associated glia, called DA-glia, which are thought to contribute to driving inflammation.
While such DA-glia were present around lesions, they also were widespread in regions of the brain and spinal cord that didn’t have lesions, the researchers discovered. These findings “support the notion that the induction of DA-glial states and the formation of lesions, although interconnected, can occur independently,” the team said.
Findings tested against postmortem samples from 6 human patients
Data indicated that some types of glia — namely microglia and astrocytes, which are known to contribute to MS-driving inflammation — tend to remain in the disease-associated state well into the late stages of EAE progression. However, another type of glial cell called oligodendrocytes tended to return to normal by the late stages of the disease.
This was particularly intriguing to the researchers because oligodendrocytes are the brain cells mainly responsible for making myelin, the fatty covering around nerve fibers that’s damaged in MS.
It’s long been assumed oligodendrocytes are mostly victims, not perpetrators, in the immune attack that drives MS — but according to Kukanja, this finding “raises the question of whether [oligodendrocytes] dampen the disease or drive it.”
Our study unveils the intricate cellular dynamics underlying MS.
After identifying these patterns in mice with EAE, the researchers applied similar in situ sequencing techniques to analyze postmortem spinal cord samples from six MS patients.
The results, overall, were consistent with the findings from mice studies; for example, the distribution of DA-glia throughout the spine was seen in human samples just as in the mice.
The team concluded that this study “provides insights into the dynamics of MS disease evolution,” adding that better understanding how cellular dysregulation leads to MS lesions may aid with “uncovering cellular and molecular pathways that may constitute novel targets for MS therapies.”
“Our study unveils the intricate cellular dynamics underlying MS,” the scientists added.