Gum disease may accelerate MS progression, mouse study suggests
Pg infection boosted pro-inflammatory pathways in immune cells in spleen
Written by |

Gum disease caused by the bacterium Porphyromonas gingivalis (Pg) is associated with worse multiple sclerosis (MS) in a mouse model of the disease, a study shows.
Infection with Pg directly or indirectly boosted pro-inflammatory pathways in immune cells in the spleen, where they’re produced, thereby aggravating MS. These effects were also associated with low oxygen conditions (hypoxia) and the activation of hypoxia-inducible factor 1 alpha (HIF-1-alpha).
The study, “Hypoxia drives progression of multiple sclerosis by enhancing the inflammasome activation in macrophages with Porphyromonas gingivalis infection,” was published in Cell Death Discovery.
In MS, immune cells abnormally launch an inflammatory attack that damages certain parts of the brain and spinal cord, causing neurological symptoms.
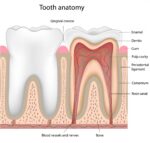
Gum disease, called periodontitis, is an infection, often caused by Pg, that leads to damage to the soft tissue around teeth. It’s been linked to several autoimmune conditions, including MS. The bacterium secretes several factors that activate the NLRP3 inflammasome, a complex of immune proteins inside cells that work as a sensor for infectious agents. When activated, the inflammasome prompts the cell to release pro-inflammatory signaling molecules that drive inflammatory responses, exacerbating tissue destruction in periodontitis.
Accumulating evidence suggests the abnormal activation of the NLRP inflammasome also contributes to the inflammation that drives MS.
Link between MS and periodontitis
Here, researchers in Japan found a possible relationship between Pg-driven periodontitis and MS.
They focused initially on low-oxygen, or hypoxic, conditions in periodontal pockets, the spaces surrounding the teeth under the gum line where these bacteria can grow.
Experiments with lab-grown mouse cells showed that, under hypoxic conditions, a Pg infection in macrophages — immune cells involved in the altered immune response that drives MS — boosts inflammasome activation. Further work revealed that certain components released by Pg increased inflammasome activation and cell death.
Looked at more closely, Pg-induced inflammasome activation under hypoxia involved signaling via TLR4, a protein on immune cells that recognizes certain bacterial molecules and triggers immune responses. In turn, TLR4 signaling activated two pathways, TRIF and MyD88.
TRIF was found to regulate the production of HIF-1-alpha, a key protein that accumulates under hypoxic conditions and activates genes to counteract low oxygen levels in the body. Further experiments showed HIF-1-alpha was crucial in accelerating macrophage inflammasome activation during Pg infection under hypoxia.
To shed light on the impact of Pg infection on MS progression, the researchers induced MS-like disease in mice after orally infecting them with either Pg or Prevotella intermedia (P. intermedia), another periodontitis-associated bacterium.
The clinical scores of the Pg-infected mice were significantly worse than those of P. intermedia-infected or uninfected mice. MS progression induced by Pg was found to be influenced by HIF-1-alpha, specifically from spleen myeloid cells, a class of immune cells that includes macrophages.
Accordingly, a lack of HIF-1-alpha in myeloid cells reversed neurological symptoms in MS mice with a Pg infection and reduced the production of pro-inflammatory signaling proteins.
“Therefore, oral Pg infection directly or indirectly activates the inflammasome in spleen myeloid cells in a [HIF-1-alpha-dependent] manner,” the researchers wrote. “However, since we could not detect Pg in the spleen after oral infection, the bacterial proteins may be transferred to the spleen via blood vessels or inflammation from oral tissues may spread [bodywide], triggering inflammasome activation.”
“Our findings indicated that hypoxia modulates inflammasome activation in response to periodontitis-related bacterial infections, contributing to the progression of autoimmune diseases,” they wrote.