First person with MS gets ‘off-the-shelf’ CAR T-cell therapy
Study testing if donor T-cells can target immune cells that drive inflammation
Written by |
A person with multiple sclerosis (MS) has for the first time been treated with an “off-the-shelf” CAR T-cell therapy called azercabtagene zapreleucel (azer-cel), a donor-derived approach that’s never before been tested in the disease.
The experimental treatment was given at Nebraska Medicine’s Fred & Pamela Buffett Cancer Center as part of a U.S.-based Phase 1 clinical trial (NCT06680037) that’s enrolling up to 32 adults with progressive forms of MS. The study is testing if genetically engineered T-cells from healthy donors can safely and effectively target the rogue immune cells that drive inflammation and damage in MS.
“This is a completely novel concept in MS therapy,” Rana Zabad, MD, a neurologist and MS specialist at Nebraska Medicine, said in a university news story. Zabad is leading the trial alongside CAR T-cell therapy expert Matt Lunning.
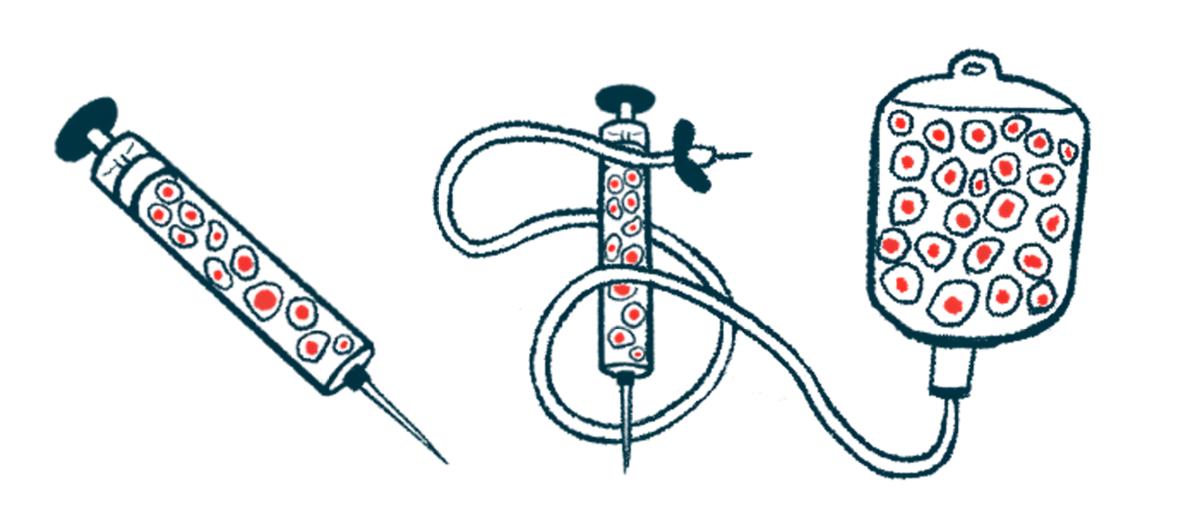
CAR T-cell therapy is a type of immunotherapy wherein immune T-cells are genetically modified to carry a man-made receptor — called a chimeric antigen receptor, or CAR — on their surface, which enables them to target a specific protein. The cells are then expanded into the millions and infused into the patient to recognize and destroy the harmful cells. Traditional CAR T-cell therapies use a patient’s own T-cells, but the manufacturing process often takes several weeks and researchers aren’t always able to collect enough cells from a patient to create the treatment.
TG Therapeutics‘ azer-cel contains T-cells from healthy donors. Termed allogeneic, or donor-derived, CAR T-cell therapy, the approach allows for the production of an “off-the-shelf” treatment that could be used in numerous patients.
“We’ve never used allogeneic CAR T-cell therapy to target the immune cells responsible for driving inflammation and damage in the central nervous system. This trial is about pushing boundaries carefully and thoughtfully to explore what could be possible,” Zabad said.
The cells in azer-cel carry a CAR that targets the CD19 protein at the surface of B-cells, immune cells that factor in driving MS. By targeting B-cells, the therapy should reduce them and ease disease symptoms.
For MS, a first of its kind
The approach has been explored in B-cell-related blood cancers, but several clinical trials are now testing both patient- and donor-derived CAR T-cell therapies in B-cell mediated autoimmune disorders.
“There is growing hope that this therapy can do more than treat patients with blood cancers like leukemia and lymphoma,” Lunning said. “A year ago, we provided the first allogeneic CAR T-cell therapy to a patient with lupus and she has seen excellent results.”
The first-of-its-kind clinical trial, which is ongoing at five sites in the U.S., will involve a round of chemo to destroy the faulty immune cells and a single infusion of azer-cel, after which patients will be followed for nearly two years.
Jan Janisch-Hanzlik, 49, was the first participant to receive the therapy and the first with MS to receive an allogeneic CAR T-cell therapy. She joined the trial after seeing her MS progress within three months, during which she could no longer drive and had to move into a new home after multiple falls.
She received the azer-cel infusion in June and was discharged a week later, returning for follow-up visits. She and other participants will be monitored to determine the treatment’s safety, its pharmacological properties, and its ability to slow disability progression and reduce lesions and brain shrinkage.
“I feel blessed that Dr. Zabad chose me for this treatment,” Janisch-Hanzlik said. “I’m not just excited for me; I’m excited for the whole MS community, including the physicians and the patients because it’s really going to help all of us in the long run.”
