Paramagnetic rim lesions could help in diagnosing MS early: Study
Areas of damage in brain, spinal cord are highly indicative of disease
Written by |
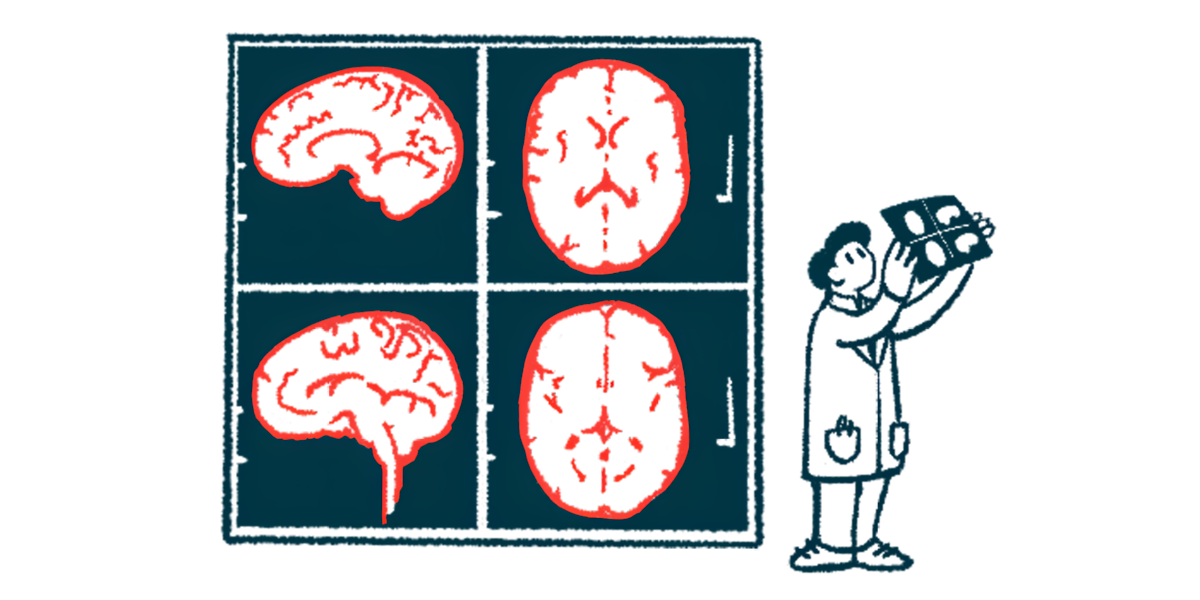
Paramagnetic rim lesions (PRLs), which represent areas of damage in the brain and spinal cord with chronic active inflammation, are highly indicative of multiple sclerosis (MS) in people being evaluated for the disease, a new study reports.
The findings support using this imaging biomarker as a useful tool for diagnosing MS, especially in people who are early in their disease course.
“PRLs are highly prevalent in people with MS initially presenting to MS clinics, and their presence differentiates early MS from other conditions with high accuracy,” Daniel Ontaneda, MD, PhD, co-author of the study at the Cleveland Clinic, said in a press release. “We used MRI sequences noninvasively acquired in a short time and employed different MRI scanners and multiple readers to detect PRLs, supporting the feasibility of using PRLs as a biomarker in clinical practice.”
The study, “Frequency and Diagnostic Implications of Paramagnetic Rim Lesions in People Presenting for Diagnosis to a Multiple Sclerosis Clinic,” was published in Neurology.
Presence of PRLs evaluated as potential imaging biomarker
MS lesions are areas of damage in the brain or spinal cord caused by the immune system attacking myelin, the protective coating around nerve fibers. Most lesions heal or stop changing after a while, but some lesions develop a thin rim that can be seen with advanced MRI scans.
This rim is made up mainly of iron-filled immune cells that remain active for years at the edge of the lesion, slowly continuing to cause damage and disability progression over time.
While MRI is essential for diagnosing MS, up to 20% of patients are still misdiagnosed. Therefore, the addition of biomarkers to the diagnostic workup could improve the rate of accurate diagnoses.
Because PRLs are rarely seen in people without MS and are estimated to occur in about 50% of MS patients, the researchers set out to evaluate if the presence of these lesions could be added as an imaging biomarker to help diagnose MS.
Patients more likely to be PRL-positive when closer to symptom onset
The team evaluated MRI data from 78 people who were evaluated for possible MS at specialty clinics between 2018 and 2020. Of them, 47% were ultimately diagnosed with MS, while the rest were diagnosed with other disorders.
The analysis revealed that 36 participants had at least one PRL. The vast majority of these patients (89%) were ultimately diagnosed with MS using the 2017 McDonald criteria, a set of guidelines that incorporate clinical and laboratory evaluations, as well as MRI data, to establish an MS diagnosis. Four patients with PRLs did not meet the criteria for an MS diagnosis, and five MS patients did not have PRLs.
This meant that the presence of PRLs had a sensitivity of 0.86 and a specificity of 0.9 for detecting MS — in other words, just looking for PRLs would accurately identify 86% of people with MS and 90% of patients without MS. Looking for two or more PRLs led to slightly better specificity, but worse sensitivity.
“We found a sensitivity of 86% and specificity of 90% when using a threshold of [at least] 1 PRL for a diagnosis of MS. These results … support the added value of PRL as a useful diagnostic imaging biomarker for early MS,” the researchers wrote.
The researchers noted that the sensitivity seen in this study was higher than other studies have reported, which they said is “most likely due to differences in cohort characteristics and imaging methods.” In particular, previous studies looking at how common PRLs are in MS patients have usually included people who were living with MS for years, not those undergoing initial diagnostic workup.
Our findings support our hypothesis that PRLs are a better indicator of MS in patients with more recent symptom onset, possibly explaining the differences in diagnostic prediction compared with earlier studies.
Statistical analyses also showed that MS patients were more likely to be PRL-positive if they were closer to the onset of symptoms. For each year that passed since symptom onset, the likelihood of having PRLs dropped by 28%. This finding lends further credence to the idea that PRLs may be most useful as a biomarker at initial diagnostic workup, the researchers said.
“Our findings support our hypothesis that PRLs are a better indicator of MS in patients with more recent symptom onset, possibly explaining the differences in diagnostic prediction compared with earlier studies,” Ontaneda said.
Ontaneda noted that, based on these and other studies, the use of PRLs as a diagnostic marker has been included in the most recent update of the McDonald criteria.