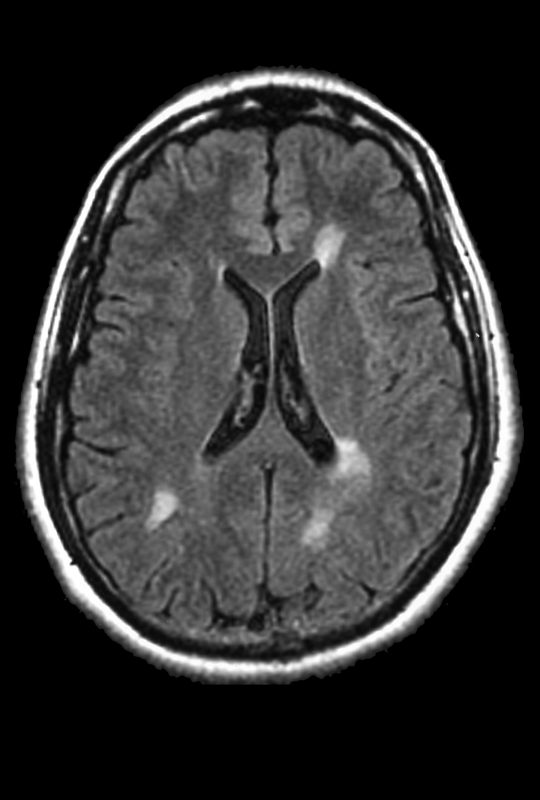
FAQs about MS brain MRI
The MRI itself usually lasts 15 to 90 minutes, depending on the specific type(s) of scan being used and which part(s) of the body may be imaged. Typically, multiple images are acquired. These images are interpreted by a radiologist, and the results are shared with the primary healthcare team and communicated to the patient. This process commonly takes a week or two, though turnaround times vary from clinic to clinic. It’s advised patients ask their healthcare providers when to expect results from MRI scans.
Contrast agents like gadolinium are typically used to detect areas of active multiple sclerosis (MS) driving inflammation on MRI scans. However, contrast agents are not needed for scans that detect any MS lesions (actively inflamed or not), so it is possible to diagnose MS without the use of these agents. It is generally recommended that, when feasible, patients should undergo scans both with and without contrast. This will help to facilitate an MS diagnosis, or not, as quickly as possible.
MRI scans of the cervical or lumbar spine — the neck and lower regions of the spinal cord, respectively — may be useful for detecting multiple sclerosis (MS) lesions in those regions. To receive a formal diagnosis of MS, a person must show evidence of lesions in at least two of four parts of the central nervous system, which include three brain regions and the spine. As such, an MRI of the spine may be useful in the diagnostic workup, but a spinal MRI alone cannot be used to diagnose MS on its own.
MRI is the gold standard for detecting and monitoring the lesions that result from myelin loss in the nervous system and define multiple sclerosis (MS). While an MRI is almost always a critical part of the diagnostic evaluation, MRIs alone are not enough to confirm the diagnosis — other tests are needed to confirm that MS-like inflammation is the cause of the damage, and to rule out other conditions that may mimic MS.
Related Articles

 Fact-checked by
Fact-checked by