Optic neuritis in multiple sclerosis
Optic neuritis is common in multiple sclerosis (MS) and is marked by inflammation that affects the optic nerve, which carries visual information from the eye to the brain.
Optic neuritis in MS can cause sudden vision problems and eye pain. It usually resolves on its own without causing permanent vision issues, though treatment may sometimes be recommended.
In MS, the immune system mistakenly attacks cells in the central nervous system, which consists of the brain and spinal cord, causing inflammation and nerve damage. When this inflammation affects the optic nerve, it results in optic neuritis.
Up to 70% of people with MS are estimated to experience optic neuritis at some point in their disease. For about 20% of patients, it is one of the first noticeable symptoms of MS, which is why optic neuritis is now included in the criteria used to establish an MS diagnosis.
While optic neuritis can have several possible causes, it is strongly linked to an increased risk of developing MS. Around half of the people who experience a first episode of optic neuritis will develop MS over the next 15 years.
Symptoms of optic neuritis
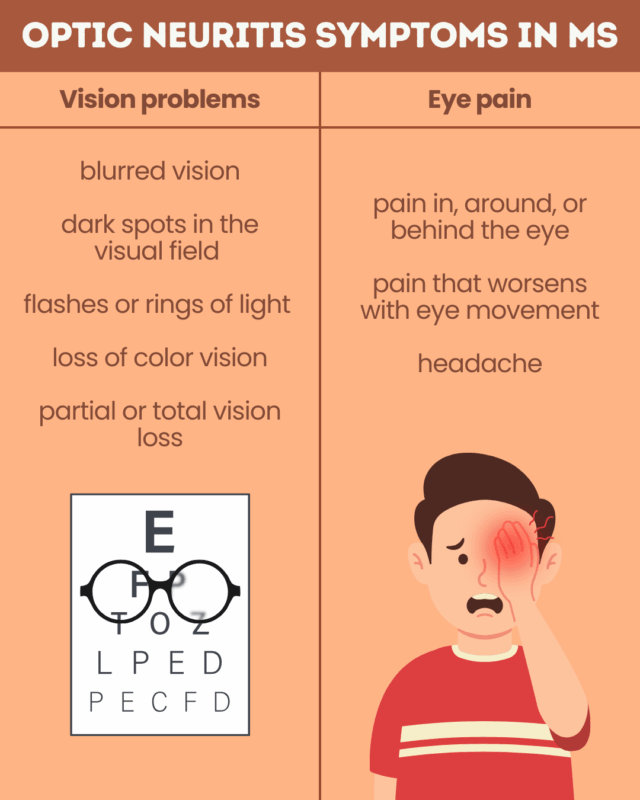
The most common symptoms of optic neuritis in MS patients are visual impairment and eye pain. Symptoms usually affect only one eye, though some people may experience optic neuritis in both eyes.
Optic neuritis can affect visual function in several ways, including:
- blurred vision
- dark spots at the center of vision
- flashes of light or rings of light (halos) in the visual field
- loss of color vision, with colors appearing dimmer or washed out
- partial or total loss of vision.
Around 90% of people with optic neuritis experience eye pain, which often worsens with eye movement. Pain in the affected eye may also radiate to surrounding areas, sometimes causing headaches behind the eye or in the front of the head.
The symptoms of optic neuritis typically develop quickly and worsen over one to two weeks. Vision problems then stabilize and usually begin to improve within two to four weeks of symptom onset.
Diagnosing optic neuritis
Optic neuritis is usually diagnosed by an ophthalmologist or neurologist through a combination of clinical exams and imaging tests that assess optic nerve damage and rule out other possible causes of vision problems.
After reviewing a person’s medical history, doctors may use:
- Visual acuity and color vision tests to evaluate the extent and nature of vision problems
- Ophthalmoscopy, which uses a light and magnifying lens to examine the back of the eye. This can show inflammation in the optic nerve.
- Pupillary light reaction test, which assesses changes in pupil size in response to light. With optic neuritis, the pupil won’t shrink as much or as quickly as in a healthy eye.
- Visual evoked potential test, which measures how quickly the brain processes visual cues. Optic nerve damage delays transmission of signals from the eyes to the brain, slowing the response time.
- Optical coherence tomography (OCT) scan, which uses high-resolution imaging to create detailed images of the back of the eye. This can detect inflammation or nerve cell degeneration consistent with optic neuritis and show early changes specific to MS.
- magnetic resonance imaging (MRI) scan of the optic nerve to look for inflammation and damage consistent with optic neuritis.
If a person has not yet been diagnosed with MS, additional tests may be used to determine whether the optic neuritis is related to the disease. These may include:
- brain MRI to detect typical signs of MS damage in the central nervous system
- blood or spinal fluid tests to identify inflammatory changes consistent with MS and rule out related conditions.
Optic neuritis treatment and outlook
Optic neuritis in MS has a generally good prognosis. Most people recover much or all of their lost vision over time, even without treatment. Much of this improvement occurs in the first month, but full recovery may take several months.
Corticosteroids, a class of anti-inflammatory medications, may be used to help accelerate recovery, particularly in more severe cases. These medications do not change the final degree of vision recovery, however, but they help symptoms resolve more quickly.
Some patients with MS may have persistent vision changes after an optic neuritis episode. More severe initial vision loss is linked to a higher chance of incomplete recovery. Studies have also suggested worse recovery in men and people who were older at disease onset.
Because MS often follows a relapsing-remitting course, marked by periods of sudden symptom worsening (relapses), a substantial proportion of patients may experience recurrent episodes of optic neuritis.
In the long term, disease-modifying therapies for MS can help reduce the risk of optic neuritis by suppressing the immune activity that drives disease relapses.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by 

