
Secondary progressive MS life expectancy
Last updated Oct. 22, 2025, by Lindsey Shapiro, PhD

Secondary progressive multiple sclerosis (SPMS) life expectancy varies widely, depending on factors such as a person’s age at onset, disease severity, overall health, and access to appropriate treatment. However, with recent advances in multiple sclerosis (MS) care, many people with SPMS now live nearly as long as those without the neurodegenerative disease.
Like other types of MS, SPMS itself is not usually fatal, though the accumulating disability that characterizes it can increase the risk of complications that may affect longevity.
Still, with consistent medical care and healthy lifestyle choices, many people with SPMS can continue to live well and maintain a good quality of life for many years.
How does SPMS progress?
Most people with MS are first diagnosed with relapsing-remitting MS (RRMS), characterized by episodes of new or worsening symptoms, called relapses, followed by periods of partial or complete recovery. Over time, some RRMS patients will transition to SPMS, in which symptoms start to progressively worsen, even in the absence of relapses.
Historically, about half of all people with RRMS would transition to SPMS within 10-20 years of disease onset. But with the availability of effective disease-modifying therapies (DMTs), this transition is being significantly delayed. A recent study found that about 10% of RRMS patients transitioned to SPMS over a median of 32 years.
The timing of this transition can have a major impact on the long-term prognosis and overall outlook for someone living with MS.
What life expectancy looks like for SPMS
On average, people with MS live about five to 10 years less than those in the general population, but this gap is narrowing with modern improvements in MS care. Overall, MS survival rates are improving, and people are now living longer with MS.
MS prognosis can differ by disease type. A 60-year Norwegian study showed that the median life expectancy was about four years shorter for people with RRMS, and about 10 years shorter for those with primary progressive MS — a form of MS where steady disability progression is observed from disease onset — compared with the general population.
Research on MS life expectancy has not definitively established where SPMS survival falls. Though SPMS life expectancy is often thought to lie between that of RRMS and PPMS, this has not been clearly confirmed in well-controlled scientific studies.
Notably, a 2025 study suggested that once the progressive stage begins, mortality rates may actually be higher in SPMS than in PPMS.
Still, the course of SPMS is highly variable, and life expectancy depends on many individual factors.
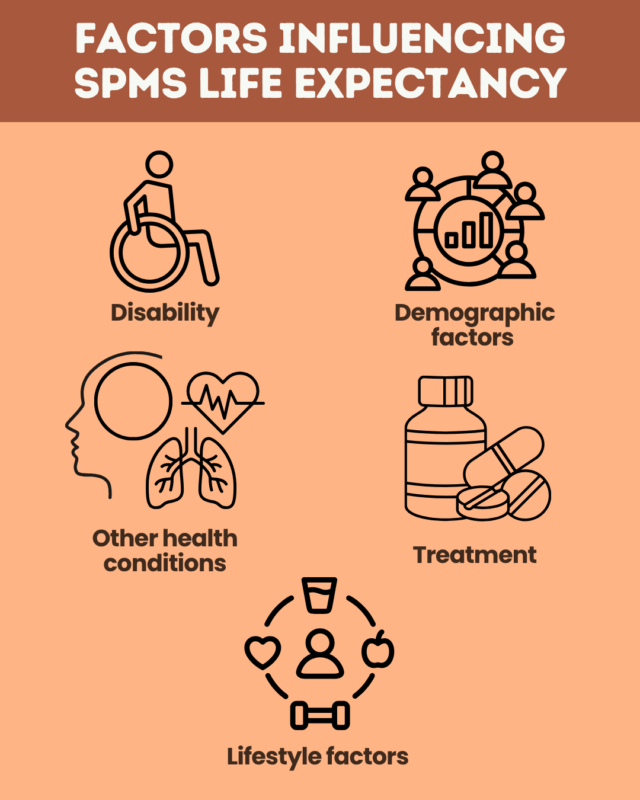
Factors that can influence life expectancy
Just as there are risk factors for developing MS, several factors can also influence SPMS prognosis.
- Disability: A greater degree of disability and faster disability progression are linked to a higher mortality risk in SPMS.
- Demographic factors: Men and people of Black or Hispanic ancestry tend to experience faster disability progression and shorter survival, while those who transition to SPMS at a younger age may live longer with progressive disability, which can increase the risk of later complications.
- Coexisting health conditions: Other health conditions, such as heart and lung disease, depression, and anxiety, are associated with faster disability progression and shorter survival.
- Treatment: Early and sustained use of MS treatments, particularly high-efficacy DMTs, can delay the transition to SPMS and slow disability progression, ultimately improving survival.
- Lifestyle factors: Maintaining good general health can improve long-term outcomes in SPMS. This may involve staying physically active, maintaining a healthy diet and weight, avoiding smoking, managing stress, and getting enough sleep.
Causes of reduced life expectancy in SPMS
SPMS itself is not usually a direct cause of death, but the increasing disability that patients experience can lead to complications that help explain the association between MS and mortality. Possible complications of SPMS include:
- Infections: Respiratory and urinary tract infections can become severe. Infections are a leading cause of death in advanced MS.
- Cardiovascular disease: People with SPMS are at a higher risk of death from heart disease or stroke, possibly due to reduced mobility with disability progression.
- Mobility-related issues: Being confined to a wheelchair or bed for long periods may lead to blood clots or pressure sores that can become serious or life-threatening.
- Suicide: The psychological burden of living with a progressive illness contributes to a higher risk of suicide among people with MS.
Many of these complications can be reduced through proactive care, including regular medical follow-up, physical rehabilitation, prompt treatment of infections, and access to psychological support.
Improving quality of life and outlook
While SPMS is progressive and increasingly interferes with daily life, many strategies can help people live better and longer with SPMS.
- Treatments for SPMS can help slow disease progression, manage symptoms, and reduce complications.
- Supportive care approaches such as physical therapy and occupational therapy can help preserve mobility and independence.
- Finding mental health support and social connection can ease the emotional burden of living with SPMS and reduce isolation.
- Adopting a healthy lifestyle can contribute to maintaining long-term health and improving quality of life with MS.
While SPMS cannot be cured, its overall outlook can be improved by working closely with a healthcare team, which will develop a personalized management plan that helps people maintain independence and quality of life with MS for as long as possible.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recommended Posts
- Starting at age 8, MS has been the invisible illness invading my life
- ‘Molecular atlas’ uses military blood samples to spot disease years early
- Living between the lines: MS, motherhood, and the invisible load
- Trial of CAR T-cell therapy for progressive MS now recruiting in US
- The ‘pre-flight safety checklist’ applies to both MS patients and caregivers




