FAQs about MS relapses
“MS relapse” and “MS flare-up” can be used interchangeably. Both refer to a sudden worsening of multiple sclerosis (MS) symptoms that cannot be explained by fever or infection. Other terms such as attack, clinical episode, and exacerbation also describe an MS relapse.
The biological causes of relapses in multiple sclerosis (MS) are not completely understood, but generally speaking, relapses are driven by new or worsening inflammation that damages nerves in the brain and spinal cord. This can interfere with nerve signals and ultimately lead to new symptoms or the worsening of older ones.
Some multiple sclerosis (MS) relapses are mild enough that they do not require treatment. Others may be severe enough to cause significant impairment and require urgent or emergency care. If patients think they are experiencing a relapse, they should contact their healthcare team to determine what to do.
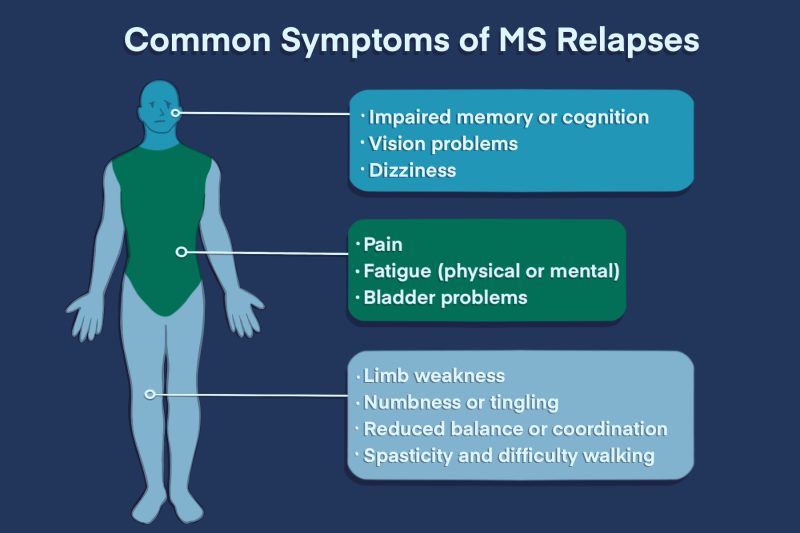
Multiple sclerosis (MS) relapses can cause any of the wide range of symptoms that may occur in MS. The specific symptoms depend on which parts of the nervous system are being actively damaged. It can be different for everyone, and even from relapse to relapse for the same person. Some of the most common relapse symptoms include fatigue, pain or other unusual sensations, weakness, spasticity, difficulty with coordination or cognition, bladder problems, and vision difficulties.
Some people with multiple sclerosis (MS) are particularly sensitive to changes in body temperature and may experience a temporary worsening of symptoms called a pseudo-relapse. While it may feel similar to an MS relapse, it is not a true flare-up because symptoms are not caused by active inflammation, and resolve once body temperature returns to normal.
Related articles

 Fact-checked by
Fact-checked by