#MSParis2017 – Researchers Suggest Propionic Acid Could Be Used as Add-on Treatment in MS
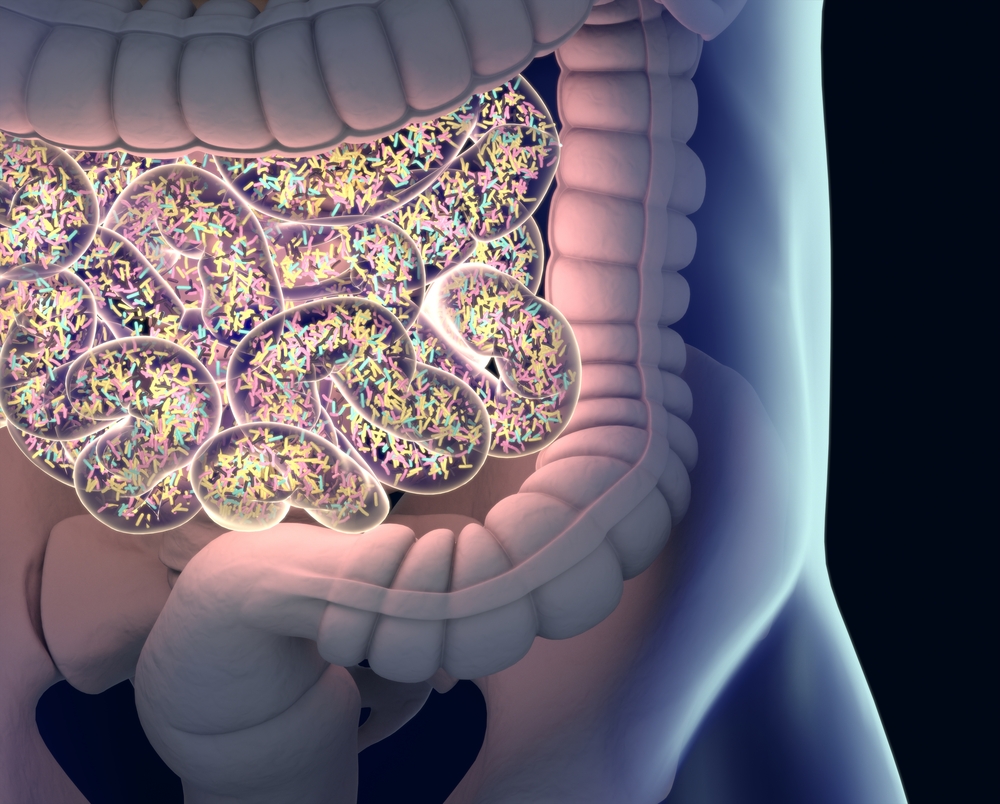
Propionic acid supplements alter the composition and behavior of immune cells in multiple sclerosis (MS) patients — likely by changing the composition of gut bacteria, according to Alexander Duscha from Ruhr University Bochum in Bochum, Germany.
The finding, presented Wednesday at the 7th Joint ECTRIMS-ACTRIMS Meeting running in Paris through Oct. 28, provides yet another piece of evidence supporting an important role for gut bacteria in modulating the immune system in MS.
The study, “Propionic acid modulates T effector cell balance and function in MS patients,” was presented at the meeting as part of the Young Scientific Investigators’ Session.
The researchers had previously studied propionic acid — a fat component produced by certain gut bacteria — in an animal model of MS. Their studies indicated that the fatty acid could slow the disease course in the animals.
They also showed that mice fed a diet rich in propionic acid also developed a richer variety of gut bacteria.
Since propionic acid is an approved food additive, the team went on to conduct a study of the compound in human MS patients.
Duscha and his colleagues recruited 90 MS patients and 30 healthy people as controls, giving them 500 mg of propionic acid twice daily for 14 to 90 days. The MS patients were all receiving various disease-modifying therapies.
After 14 days, they noted a drop in inflammatory T-cell numbers in both patients and controls, but with a more pronounced reduction in MS patients. Meanwhile, the number of regulatory T-cells, or Tregs, increased by 30 percent.
Tregs are important cells that prevent autoimmune reactions, and according to Duscha, the “suppressive capacity of Tregs in MS is diminished by 20 percent.”
Researchers also noted that Tregs were better at modulating immune responses after propionic acid treatment in MS patients. “After only 14 days of propionate treatment, the suppressive capacity [of Tregs] was highly increased,” Duscha said.
Analyzing the types of gut bacteria in MS patients and controls, the team noted significant differences, particularly with relapsing-remitting MS (RRMS) patients having a lower diversity of gut bacterial types.
“Microbiome analysis on stool samples demonstrates differences between MS and healthy controls, but also between RRMS and primary progressive (PPMS) and secondary progressive MS (SPMS) in terms of variability, both before and after treatment.”
Regarding safety, patients did not report any side effects of propionic acid treatment during the study.
Overall, the study’s results indicate that the findings in mice are also valid in people with MS, and suggest propionic acid could be a valuable supplement to be used as an add-on therapy to disease-modifying drugs.






