Australian Researchers Identify Master Regulator of the Faulty Inflammation Signaling in MS
Australian researchers have identified the master regulator of the immune response signaling pathway that is out of sync in multiple sclerosis and other inflammatory diseases.
The lynchpin in the process is the xIAP protein, the team said. Their discovery that it triggers the NOD2 pathway’s faulty inflammation signaling could lead to new therapies for MS.
Their study, “IAPs Regulate Distinct Innate Immune Pathways to Co-ordinate the Response to Bacterial Peptidoglycans,” appeared in the journal Cell Reports.
Another protein, NOD2, also helps control the signaling pathway. But xIAP plays a larger role, the team said.
Defects in the signaling pathway lead to MS and the bowel disease Crohn’s, whose hallmarks include uncontrolled inflammation.
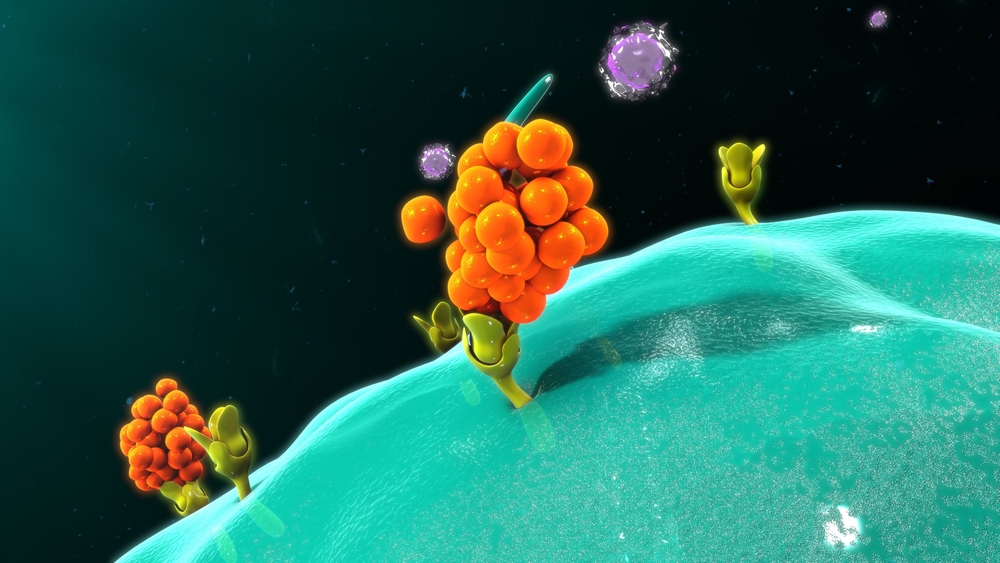
When the NOD2 pathway is working as it should, it detects invaders such as bacteria, triggering the release of inflammatory signals to fight the infection. But defects in the pathway’s control system lead to immune cells continuing to generate inflammation after an infection is cleared. The result is a chronic inflammatory disease.
“Inflammation occurs when our immune cells release inflammatory messengers, or cytokines, which is a normal response to disease,” Ueli Nachbur of the Walter and Eliza Hall Institute of Medical Research said in a press release. “However when too many cytokines are produced, inflammation can get out of control and damage our own body — a hallmark of inflammatory diseases,” said Nachbur, the co-lead author of the study.
The researchers were intent on identifying the master regulator of the inflammation that the NOD2 pathway triggers.
They determined that the xIAP protein “was the key to initiating the inflammatory response in these cells,” said Che Stafford, the study’s first author. “We also showed that, once the NOD2 pathway trigger is initiated, the cells need a second, amplifying step to complete a full-strength immune response.”
Identifying both what triggers the inflammation signaling, and what strengthens it, were necessary to laying the groundwork for a therapy, the team said.
“Targeting key components of the NOD2 pathway shows promise as a way of switching off ongoing inflammation associated with diseases such as Crohn’s disease and multiple sclerosis,” Stafford said. In 2015 the team used preclinical-trial studies to show “that blocking a different protein in the NOD2 pathway could halt inflammation, and was able to halt the progression of multiple sclerosis,” he said. “So it is very exciting to identify other potential targets for treating these diseases.”
“xIAP has other roles in the cell, such as regulation of cell death, so it is a tricky target for treating inflammatory diseases,” Nachbur said. “However these new discoveries provide us with vital information to develop new treatment strategies that could lead to a safe and effective way of switching off inflammation for treating disease.”






