Study Links Food Allergies and Increased MS Disease Activity
Multiple sclerosis (MS) patients who reported food allergies showed a 27 percent higher cumulative rate of flare-ups over the course of their disease, and more than twice the likelihood of having active inflammatory lesions, a new study shows.
The study, “Food Allergies are Associated with Increased Disease Activity in Multiple Sclerosis,” led by researchers at Partners MS Center, Brigham and Women’s Hospital at Harvard Medical School, was published in the Journal of Neurology, Neurosurgery & Psychiatry.
Several genetic and environmental factors have been associated with MS development.
Allergy to environmental triggers (like pollen, grass, or dust mites), certain medicines, or food (like nuts, shellfish, or wheat) have been suggested as potential risk factors for the disease. However, the data available so far have been inconclusive.
To determine whether there is an association between MS and allergy, researchers assessed 1,349 individuals with MS enrolled in the Comprehensive Longitudinal Investigation of Multiple Sclerosis at the Brigham and Women’s Hospital (CLIMB) study. The average disease duration of the patients was 16 years.
Participants completed a self-administered questionnaire about environmental, medicinal, and food allergies.
Among participants, 427 had no known allergies; 922 had one or more allergies. Allergic patients were divided into three groups: those suffering from environmental allergies (586 patients), from food allergies (238), or from allergies associated with prescribed medication (574).
Join the MS forums: an online community especially for patients with MS.
Researchers collected data on the total number of MS flare-ups/relapses each participant had experienced over the course of their disease, and data concerning their expanded disability status scale (EDSS), MS severity score (MSSS), and magnetic resonance imaging (MRI) scans. The MRI parameters analyzed were the presence and number of lesions detected. All these measures are indicative of the patient’s disease activity.
After statistically adjusting for other factors that could influence the outcome, results showed that patients reporting food allergies had a cumulative number of relapses that was 27 percent higher than patients with no known allergies.
In addition, patients in the food allergy group showed more than twice the likelihood of having lesions on MRI scans. In contrast, the environmental and medication allergy groups did not show significant differences when compared to those without allergies.
The EDSS and MSSS scores were not affected by any type of allergy.
Although this was an observational study, which cannot unambiguously establish a cause-and-effect relationship, it suggests a possible association between food allergies and MS flare-ups, the team noted.
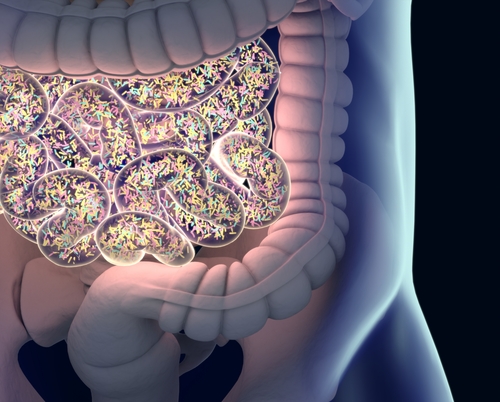
The fact that other types of allergies did not show this association supports the idea that there may be a specific link between gut bacteria and the immune system or neurological diseases.
“Our findings suggest that MS patients with allergies have more active disease than those without, and that this effect is driven by food allergies,” the researchers concluded, according to a press release.
The team proposed two explanations. Food allergies may trigger inflammation of the gut mucosa, which enhances disease activity, or they may change the gut bacteria, creating neuro-active chemicals that affect the central nervous system.
More studies are needed to confirm the findings, researchers said, to determine the underlying biological mechanisms of the association between food allergies and MS disease activity.






