FAQs about Copaxone
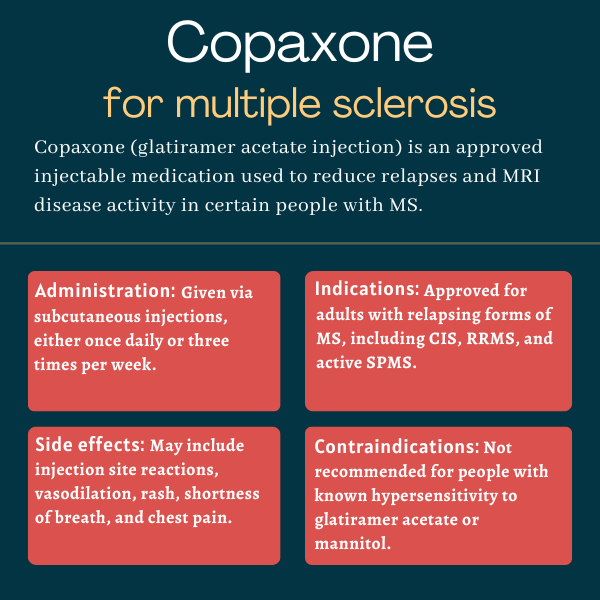
Copaxone was initially approved by the U.S. Food and Drug Administration in December 1996 for the daily treatment of adults with relapsing-remitting multiple sclerosis (MS). The label was later expanded to also include other forms of relapsing MS. A different formulation of the medication that’s injected less frequently was approved in 2014.
According to animal data and findings from observational clinical studies, Copaxone use during pregnancy does not harm a developing fetus. However, there haven’t been any well-controlled studies in pregnant women. Patients are advised to inform their healthcare team if they are pregnant or have plans to become pregnant while on Copaxone.
No known interactions exist between Copaxone and alcohol. However, given that alcohol can interfere with some medications and disease symptoms, patients should discuss the topic with their healthcare providers.
According to Copaxone’s developer, Teva Pharmaceuticals, patients using the medication may see results after one year. However, responses to treatment can vary. Patients should talk with their healthcare team about how Copaxone is expected to help in their case.
Weight gain and hair loss were not reported in clinical trials as common side effects of Copaxone, but there are some isolated reports of weight gain or weight loss. Patients who experience unanticipated effects from treatment should discuss them with their healthcare team.
 Fact-checked by
Fact-checked by