FAQs about prednisone
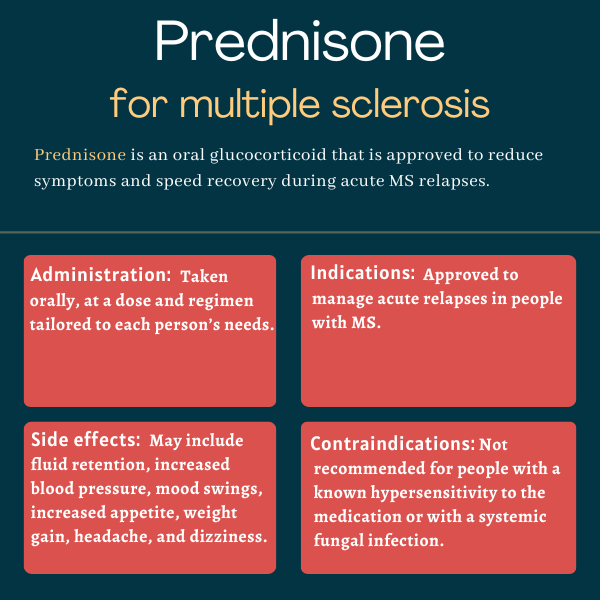
Prednisone is a glucocorticoid that is used to manage relapses, or times when new symptoms suddenly appear or older ones worsen, in people with multiple sclerosis. It works by reducing the inflammation that drives relapses, thus helping to alleviate symptoms and shortening the duration of relapses. Prednisone, however, does not alter the long-term progression of the disease.
Prednisone may cause harm to a developing fetus and should only be taken during pregnancy if the potential benefits outweigh the risks. These should be discussed in detail between patients and their healthcare providers when deciding if prednisone could be an option.
Alcohol is not known to directly interact with prednisone. However, prednisone and alcohol can cause similar effects on the body, so alcohol may increase the chances of experiencing certain side effects from the medication. Patients receiving prednisone should ask their healthcare team about safe alcohol consumption during treatment.
It is difficult to predict when and if people with multiple sclerosis will respond to treatment with prednisone. However, most people experience initial improvements within several days to weeks, with continued improvement being observed for up to six months in some cases. [from here]
An increase in appetite and weight gain are common side effects of prednisone treatment. Though less common, thinning of hair on the scalp is also a potential side effect of treatment with prednisone. Patients should talk with their doctor about any side effects they experience while on treatment.
 Fact-checked by
Fact-checked by