New MRI Study Shows Strong Correlation Of Gray Matter Myelin Loss To MS Disability
Written by |
Loss of myelin, the fatty protective sheath around nerve fibers, is a characteristic of multiple sclerosis (MS). A new magnetic resonance imaging (MRI) study by a team of researchers has determined that people with MS lose myelin in the gray matter of their brains, and that the amount of loss is closely correlated with symptom severity. In an original research paper published online, September 10, in the journal Radiology, the scientists report that they found gray matter demyelination much more advanced in patients with secondary-progressive MS, and very strongly related to a patient’s degree of disability.
The Radiology paper, entitled “Fast Whole-Brain Three-dimensional Macromolecular Proton Fraction Mapping in Multiple Sclerosis“ (Published online ahead of print: September 10, 2014; Radiology, doi:10.1148/radiol.14140528) is coauthored by Vasily L. Yarnykh, PhD and Kenneth R. Maravilla, MD of the Department of Radiology, at the University of Washington in Seattle; James D. Bowen, MD, Pavle Repovic, MD, Angeli Mayadev, MD, Peiqing Qian, MD, Beena Gangadharan, PhD, and Lily K. Jung Henson, MD of the Multiple Sclerosis Center and Bart P. Keogh, MD, PhD, of the Department of Radiology at the Swedish Neuroscience Institute, Seattle, Wash; and Alexey Samsonov, PhD, of the Department of Radiology, University of Wisconsin, Madison, Wisconsin.
The scientists note that whole-brain macromolecular proton fraction mapping enables quantitative assessment of demyelination in normal-appearing white and gray matter, and better correlates with clinical status in multiple sclerosis than traditional magnetization transfer and R1 mapping.
 While MS is typically considered a disease of the brain’s signal-conducting white matter, where myelin is most abundant, myelin is also present in smaller amounts in gray matter, the brain’s information processing center consisting primarily of nerve cell bodies. Even though myelin content in gray matter is small, it is still extremely important to proper function, since it enables protection of thin nerve fibers connecting neighboring areas of the brain cortex, according to Vasily L. Yarnykh, Ph.D., — a study coauthor and an associate professor in the Department of Radiology at the University of Washington in Seattle.
While MS is typically considered a disease of the brain’s signal-conducting white matter, where myelin is most abundant, myelin is also present in smaller amounts in gray matter, the brain’s information processing center consisting primarily of nerve cell bodies. Even though myelin content in gray matter is small, it is still extremely important to proper function, since it enables protection of thin nerve fibers connecting neighboring areas of the brain cortex, according to Vasily L. Yarnykh, Ph.D., — a study coauthor and an associate professor in the Department of Radiology at the University of Washington in Seattle.
“The fact that MS patients lose myelin not only in white but also in gray matter has been proven by earlier post-mortem pathological studies,” says Dr. Yarnykh in a Radiological Society of North America release. “However, the clinical significance of the myelin loss, or demyelination, in gray matter has not been established because of the absence of appropriate imaging methods.”
The coauthors report that this institutional review board approved and HIPAA-compliant study’s objective was to evaluate the clinical utility of fast whole-brain macromolecular proton fraction (MPF) mapping in MS and compare MPF with established quantitative magnetic resonance (MR) imaging measures of tissue damage including magnetization transfer (MT) ratio and relaxation rate (R1).
[adrotate group=”4″]
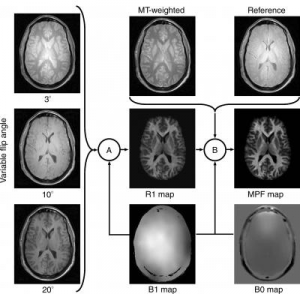
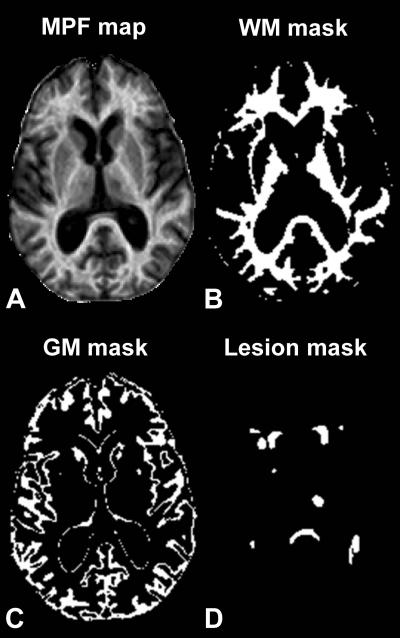
Photo Caption: The scheme demonstrating how an MPF map is computed from source MR images. Imaging protocol includes three gradient-echo images with variable flip angles, a gradient-echo image with off-resonance radiofrequency saturation enabling the magnetization transfer effect (MT-weighted image), and a reference image that is a similar gradient-echo image obtained without saturation. Additionally, an MR imager produces maps of the main magnetic field (B0) and radiofrequency field (B1), which are used to correct errors caused by imperfectness of imager’s hardware. MPF maps are computed voxel-by-voxel in two steps, (A) and (B), using special software developed by the authors. During the first step (A), a map of the longitudinal relaxation rate (R1) is generated as described in the literature. This map along with an MT-weighted image and a reference image are used to compute an MPF map in the second step (B) based on an iterative algorithm recently described by the authors. – Image Credit: Radiological Society of North America
To learn more about associations between MS and demyelination in both white and gray matter, Dr. Yarnykh and his colleagues used a refined MRI technique that provides information on the content of biological macromolecules molecules present in tissues and composed of a large number of atoms, such as proteins, lipids and carbohydrates. The new method, known as macromolecular proton fraction (MPF) mapping, has been hampered in the past because of the length of time required for data collection, but improvements now allow much faster generation of whole-brain maps that reflect the macromolecular content in tissues.
“The method utilizes a standard MRI scanner and doesn’t require any special hardware — only some software modifications,” Dr. Yarnykh observes. “MPF mapping allows quantitative assessment of microscopic demyelination in brain tissues that look normal on clinical images, and is the only existing method able to evaluate the myelin content in gray matter.”
The researchers enrolled 30 MS patients, including 18 with relapsing-remitting MS (RRMS), the most common type of MS initially diagnosed, and 12 with the more advanced type of disease known as secondary progressive MS (SPMS). Fourteen healthy control participants were also included in the study. Each participant underwent MRI on a 3-Tesla imager, and the researchers reconstructed 3-D whole-brain MPF maps to look at normal-appearing white matter, gray matter and MS lesions. The researchers further compared the results of their imaging technique with clinical tests characterizing neurological dysfunction in MS patients.
The scientists found that RRMS patients had lower white matter and grey matter MPF than controls, and that EDSS and MSFC demonstrated strongest correlations with MPF in grey matter. They conclude that MPF mapping enables quantitative assessment of demyelination in normal-appearing brain tissues and shows primary clinical relevance of GM damage in MS. Additionally, MPF outperforms MT ratio and R1 in detection of MS-related tissue changes.
The study results showed that MPF was significantly lower in both white and gray matter in RRMS patients compared with healthy controls, and was also significantly reduced in both normal-appearing brain tissues and lesions of SPMS patients compared to RRMS patients with the largest relative decrease in gray matter. MPF in brain tissues of MS patients significantly correlated with clinical disability and the strongest associations were found for gray matter.
“The major finding of the study is that the loss of myelin in gray matter caused by MS in its relative amount is comparable to or even larger than that in white matter,” says Dr. Yarnykh. “Furthermore, gray matter demyelination is much more advanced in patients with secondary-progressive MS, and it is very strongly related to patients disability. As such, we believe that information about gray matter myelin damage in MS is of primary clinical relevance.”
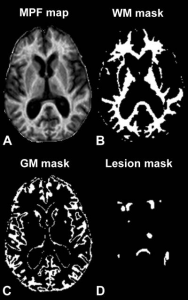
Photo Caption: These are example axial sections of a three-dimensional MPF map (A) obtained from a 63-year old woman with SPMS disease course and results of brain tissue segmentation (B-D). Segmentation masks corresponding to white matter (WM) (B), gray matter (GM) (C), and lesions (D) were used to calculate mean MPF values in each tissue. – Image Credit: Radiological Society of North America
“First, this method may provide an objective measure of the disease progression and treatment success in clinical trials,” Dr. Yarnykh observes. “And second, assessment of both gray and white matter damage with this method may become an individual patient management tool in the future.”
Dr. Yarnykh and colleagues are currently conducting additional research on the new method with the support of the National Multiple Sclerosis Society and the National Institutes of Health
“This study was done on the participants at a single point in time,” Dr. Yarnykh notes. “Now we want to compare MS patients with control participants to see how myelin content will evolve over time. We further plan to extend our method to the spinal cord imaging and test whether the combined assessment of demyelination in the brain and spinal cord could better explain disability progression as compared to brain demyelination alone.”
The Oak Brook, Ill. based Radiological Society of North America, Inc. (https://radiology.rsna.org/) is an association of more than 53,000 radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation.
Sources:
Radiological Society of North America
Radiology
The University of Washington
Image Credits:
Radiological Society of North America
The University of Washington