CONy16: MS Researchers Question Possible Long-term Benefits of Remyelination Therapies
Written by |
Multiple sclerosis was a main focus at the four-day 10th World Congress on Controversies in Neurology (CONy), in Lisbon, Portugal, that concluded on March 20. Among the topics of debate was demyelination as the disease’s main pathogenic precursor and the clinical potential of remyelination.
The debate, titled “Can we expect long-term clinical improvement through remyelination?” and hosted by David Leppert from Roche, in Basel, Switzerland, included the views of Abhijit Chaudhuri from Queen’s Hospital, U.K., and Olaf Stuve from the University of Texas Southwestern Medical Center. It focused on demyelination and neurodegeneration linked to clinical disability, and a possible combination of the two mechanisms.
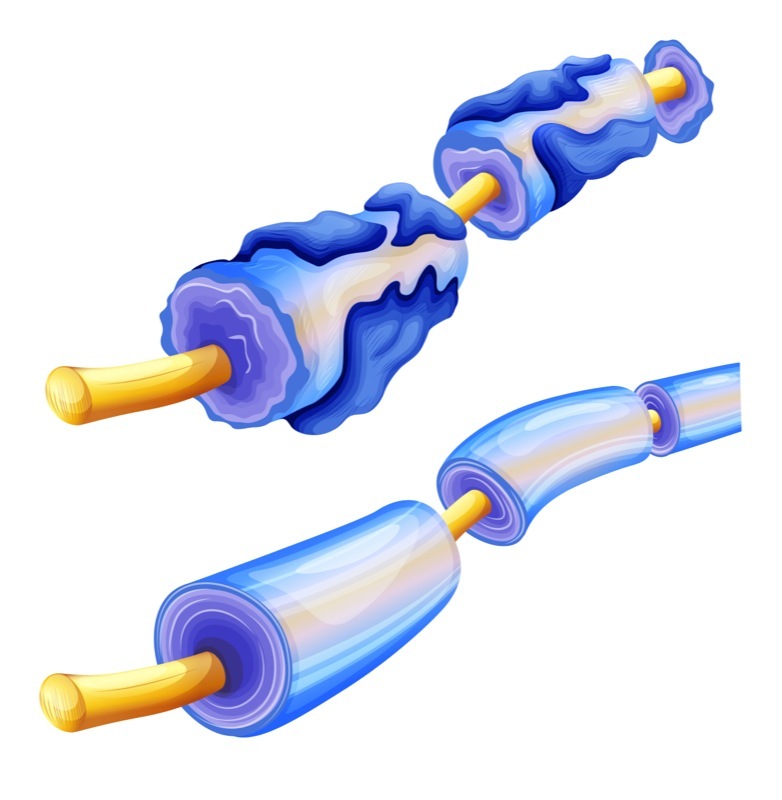
Demyelinating plaques, with surrounding inflammation and neurodegeneration, are hallmarks common to all types of MS. Despite being one of the key pathological changes in the disease, a demyelination-specific autoimmune reaction has never been identified, and the precise cause for MS remains unknown, mainly due to the complexity of the disease.
Myelin loss leads to a progressive decrease of nerve conduction velocity, and to a higher predisposition of axons to neurodegeneration due to the lack of physical and metabolic support. Dr. Stuve’s argued that myelin damage and axonal loss are the core of neurological disability in MS, a position he supported by noting that axonal loss can be detected in the earliest stages of MS, and that brain atrophy, assessed by magnetic resonance imaging (MRI), is evident in MS patients with different disease phenotypes and degrees. Both mechanisms, in their different degrees of severity, are likely irreversible and, as such, he said, remyelination strategies are unlikely to show much efficacy in recovering MS patients’ neurological abilities.
Dr. Chaudhuri highlighted remyelination events, which are characteristic of relapsing-remitting MS. He noted that spontaneous remyelination in MS lesions is either limited to the lesions’ edge or occurs throughout the entire lesion region, forming the so-called “shadow plaques,” but these remyelinated plaques may become future targets of demyelination. Moreover, there is no evidence of positive correlation between the number of shadow plaques or early remyelination and better functional preservation in patients with any type of MS.
MS research has focused on the development of novel drugs targeting pathways that promote remyelination, but existing evidence suggests that none of these agents promote remyelination beyond the naturally occurring levels.
In light of this evidence, Dr. Chaudhuri argued that attempts at remyelination would be, at best, partial or incomplete, and this treatment strategy alone would not yield meaningful functional improvements or axonal rescue and reverse neuronal loss. This failing would be even more evident if the theory that MS is primarily a neurodegenerative disease, and loss of myelin a secondary effect, was proven to be true. The scientist theorized that the benefit of remyelination would likely be improvement of nerve conduction, instead of grey and white matter protection from progressive MS pathology.
Dr. Chaudhuri concluded that, at this point, long-term clinical improvement from remyelination therapy is purely speculative, due to the lack of robust clinical data and the yet-to-be-identified appropriate imaging marker of remyelinating lesions in MS.


