Researchers Identify 2 Cytokines Responsible for Chronic Flares in Autoimmune Diseases
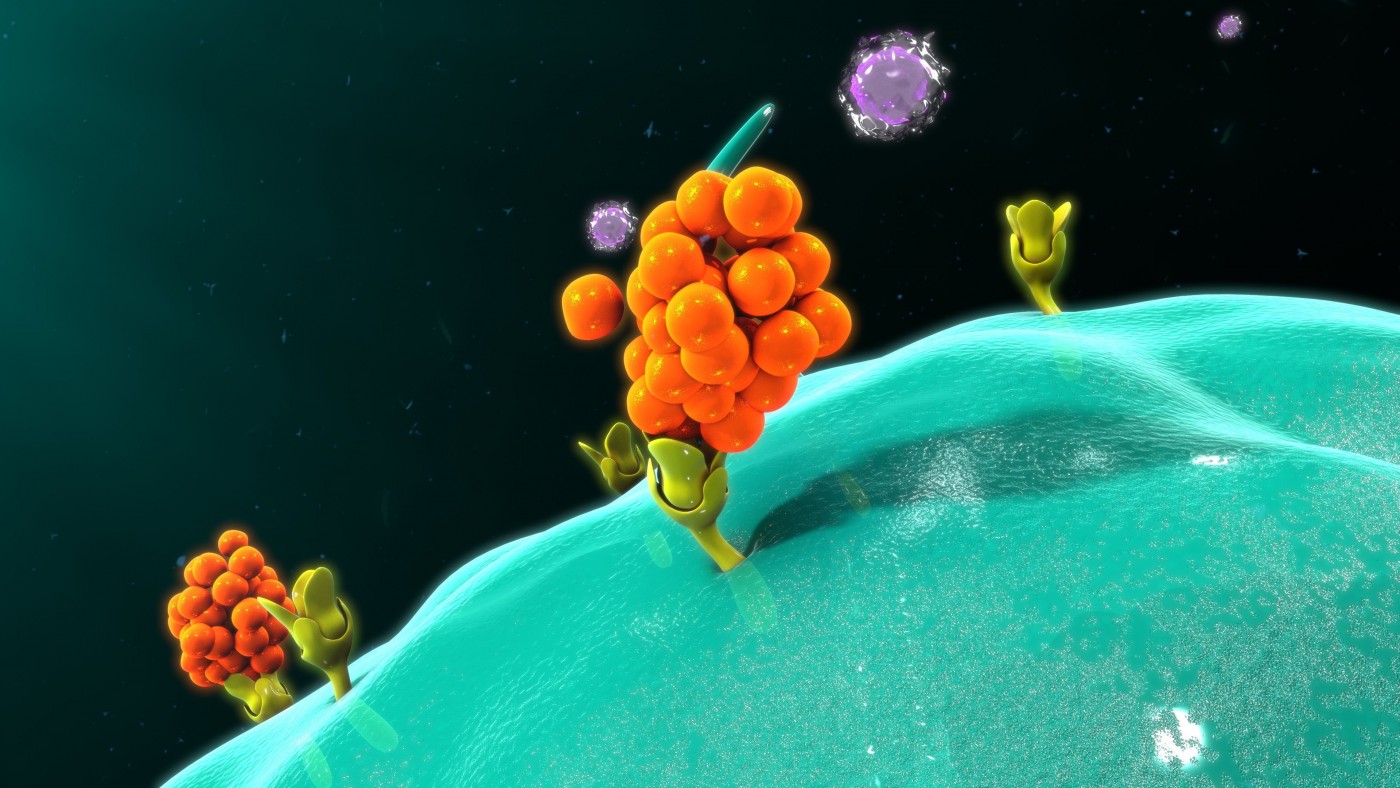
Researchers have identified two factors that allow Th17 cells — which drive multiple sclerosis (MS) and other autoimmune conditions — to form memory cells in the body and cause repeated symptom flare-ups.
Knowing the identity of the molecules, which are immune mediators called cytokines, will make it possible for scientists to search for ways to prevent T-cells from entering a chronic state.
“Interleukin-7 and -15 maintain pathogenic memory Th17 cells in autoimmunity” was published in the Journal of Autoimmunity.
More and more research points to Th17 T-cells as being responsible for the chronic nature of autoimmune diseases. In such conditions, a subset of T-cells form memory cells, and they circulate in the body and cause recurrent symptom flares. Scientists have yet to determine the events that cause the memory cells to form.
A research team from Schepens Eye Research Institute of Massachusetts Eye and Ear decided to take a closer look at the cytokines interleukin-7 (IL-7) and -15 (IL-15). Recent studies have suggested that they might be involved in autoimmune conditions.
By blocking IL-7 and IL-15 in a mouse model of the autoimmune dry eye disease, the researchers realized that these cytokines are crucial for Th17 cells’ survival. Without them, substantially fewer memory cells formed.
“We wanted to know the precise factors that maintain memory in Th17 cells so that we can better understand what is causing chronic autoimmune disorders,” Reza Dana, MD, director of the Cornea and Refractive Surgery Service at Massachusetts Eye and Ear, said in a press release.
The finding could be significant if researchers can find a way to translate it into treatments for human autoimmune diseases.
“By selectively targeting the production and expression of IL-7 and IL-15, we may be able to prevent the development of chronic autoimmune disorders,” said Dana, who also is the Claes H. Dohlman Professor of Ophthalmology at Harvard Medical School. “In the case of dry eye disease, many of the treatments are showing limited efficacy in patients that do not have a highly inflamed eye. Targeting the chronic, immune nature of autoimmune diseases may be a better strategy for controlling these conditions.”






