Cellular Metabolism Could Be New Therapeutic Target in MS, Study Suggests
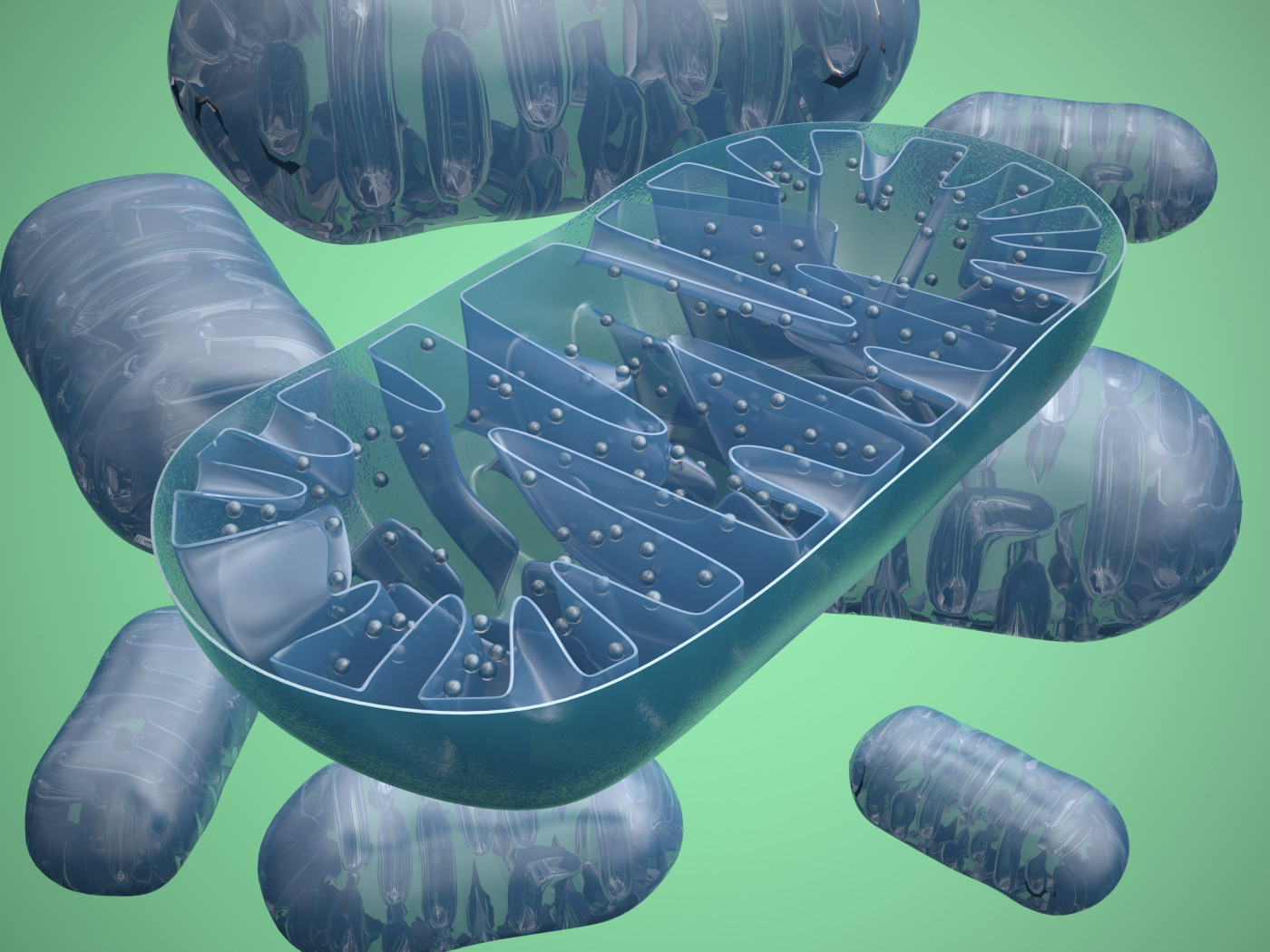
Immune system cells can either trigger or suppress inflammation by controlling mitochondrial respiration — the process that occurs in mitochondria, the cells’ powerhouses, and results in the production of usable energy by cells — according to a recent study.
This discovery raises the possibility that manipulating cellular metabolism could become a therapeutic approach for treating autoimmune disorders, allowing the balance between the types of immune cells to be controlled, the researchers say.
The study, “Mitochondrial Oxidative Phosphorylation Regulates the Fate Decision between Pathogenic Th17 and Regulatory T Cells,” was published in the journal Cell Reports.
People with multiple sclerosis (MS) and other inflammatory autoimmune diseases have an imbalance between the immune cells that trigger inflammation and those that moderate it.
Th17 cells are immune T-cells that mediate chronic inflammation, and are often elevated in autoimmune disorders. Conversely, regulatory T -cells, or Treg cells, suppress inflammatory responses and are typically diminished in patients with autoimmune diseases.
Both Th17 cells and Treg cells begin as naïve CD4 T-cells, a precursor cell. At a certain point in their development, however, CD4 T-cells receive signals that induce them to adopt either inflammatory or regulatory properties, a process called differentiation.
At the beginning of the signaling cascade that leads to differentiation, T-cells undergo a profound shift in their metabolism. In particular, they increase their rates of glycolysis (which breaks down glucose) and mitochondrial oxidative phosphorylation (OXPHOS). This allows them to meet the greater demand for energy needed for the differentiation process.
Glycolysis and OXPHOS are two processes that cells use to obtain energy from stored molecules.
It is known that fully differentiated Th17 cells show more mitochondrial respiration in comparison with naïve CD4 T-cells. But the precise contribution that OXPHOS makes to the Th17 fate has not been well-defined.
Understanding how this works raises the possibility of being able to manipulate the process, and therefore control the balance between the two immune cell types.
Thus, a team led by researchers at University of Alabama at Birmingham (UAB) used a mouse model of MS — called experimental autoimmune encephalomyelitis, or EAE — to further study the relationship between mitochondrial OXPHOS and Th17 differentiation.
CD4 T-cells taken from EAE mice were treated with either an inert control or with oligomycin — an inhibitor of mitochondrial OXPHOS. The cells were then transferred back into mice, which were monitored for the onset and severity of disease symptoms.
The results showed that mice given T-cells treated with oligomycin showed a significant delay in disease onset and reduced severity. That suggested that mitochondrial respiration is needed for Th17 cells to promote inflammation.
The T-cells that resulted from mitochondrial OXPHOS inhibition showed much in common with inflammation-reducing Treg cells. Similarities included various active genes, and the inability to activate STAT3 and BATF, two key cell fate-determining molecules in Th17 differentiation.
Interestingly, the researchers found that inhibiting mitochondrial OXPHOS in the first 24 hours of differentiation was enough to lock the cells into a Treg-like fate.
“Inhibition of mitochondrial OXPHOS ablates Th17 pathogenicity in a mouse model of multiple sclerosis and results in generation of functionally suppressive Treg cells under Th17 conditions,” Laurie Harrington, PhD, professor at AUB and the study’s lead author, said in a news story.
Overall, the study demonstrated the profound way in which mitochondrial metabolism can guide cellular differentiation.
“Our study highlights the possibility that manipulating cellular metabolism, and specifically mitochondrial OXPHOS, may provide a new promising therapeutic intervention for modulating the balance between pathogenic Th17 and Treg cells in chronic autoimmune disorders,” the researchers said.






