Rim Lesions, Suggesting Chronic Inflammation, May Be Common
Written by |
An imaging feature called a rim lesion is found in about 4 out of every 10 people with multiple sclerosis (MS), according to a review study.
These rims, thought to represent areas of chronic brain inflammation in which myelin is being progressively damaged, may serve as alternate biomarkers of disease progression and likely patient outcomes.
Its researchers recommended that “clear guidelines” be introduced to standardize how rim lesions are assessed.
Results were in the study “The prevalence of paramagnetic rim lesions in multiple sclerosis: A systematic review and meta-analysis,” published in PLOS One.
In MS, the immune system launches an inflammatory attack in the brain, leading to demyelination — the loss of the myelin sheath that surrounds neurons (nerve cells) and is critical for their function.
Brain inflammation, and the damage it causes, can be visualized using imaging technologies like MRI. Understanding exactly how imaging features correlate to aspects of disease in MS is an area of ongoing study.
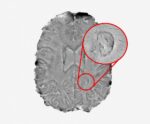
Researchers at the University of Edinburgh in the U.K. focused on a specific imaging feature called a “rim lesion.” As its name suggests, this is a feature occurring at the edge of a lesion, which can sometimes be seen when imaging using susceptibility-based MRI.
“Susceptibility-based MRI is a relatively recent addition to the MS imaging research toolbox, and there is currently considerable variation” in how it’s interpreted, the researchers wrote.
Rim lesions might be reflective of the activity of immune cells like microglia and macrophages, so they may “reflect chronic inflammatory demyelination in MS patients,” the team added. However, little is known about these imaging features in MS.
To gain more insight, the researchers conducted a meta-analysis — a type of scientific study where scientists analyze pooled data from multiple, previously published studies. Since they rely on data from many different studies, meta-analyses generally have more statistical power than individual studies.
In total, the team assessed 29 studies with data on 1,230 people; the number of patients in each study ranged from five to 294. Patients had a mean age range of 32 to 54.1, while their average disease duration ranged from 1.5 to 17 years.
All MS types were represented, with the most common being relapsing-remitting disease (RRMS).
The meta-analysis showed that rim lesions were found in roughly 40% of these MS patients, and the “rim” feature was found in about 1 out of every 10 (9.8%) lesions. The researchers noted, however, that there was “considerable” variation study-to-study.
“Our systematic review suggests that paramagnetic rim lesions are present in a substantial proportion of MS patients, notwithstanding considerable heterogeneity [variation],” the team wrote.
This variation was due to differences in study populations, and in MRI examination criteria, supporting a “need to establish clear criteria for evaluation of rim lesions, which will improve interpretation of data acquired across different research centres,” the researchers wrote. Such criteria “will allow validation and potential translation of this imaging marker into future clinical practice.”
People who were older, or who had been living with MS for a longer time, tended to have significantly fewer rim lesions, statistical analyses showed.
“The prevalence of rim lesions on a per-lesion basis was significantly lower in studies involving older patients or patients with longer disease durations. However, factors such as MRI sequence, gender and [disability], did not appear to influence the prevalence observed across studies,” the researchers wrote.
This finding “could reflect more widespread inflammatory activity during early stages of the disease,” they added, stressing that more research is needed.