Gut bacteria may be key to activate immune cells that trigger MS
New mouse study findings may lead to therapy options in long term
Written by |
Pro-inflammatory immune cells that can target the brain may be activated in a specific region of the intestine by certain gut bacteria before migrating to the brain, according to a new study done in mice.
Researchers say these findings provide a proof of concept for how some immune cells may become activated to trigger the inflammatory attack on the brain and spinal cord that causes multiple sclerosis (MS).
“Our results make an important contribution to better understanding the development of multiple sclerosis and potentially open up new therapy options in the long term,” Naoto Kawakami, PhD, the study’s senior author from the University of Munich Hospital, in Germany, said in a university press release.
The study, “Visualizing the activation of encephalitogenic T cells in the ileal lamina propria by in vivo two-photon imaging,” was published in the journal PNAS.
What is the role of gut bacteria in triggering MS?
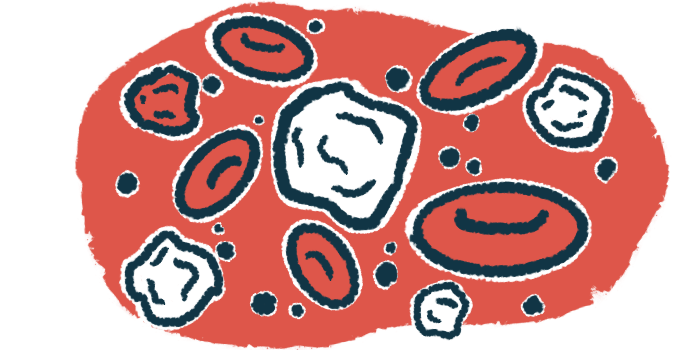
T-cells are a type of immune cell with key roles in controlling inflammation. Each T-cell is equipped with a specialized receptor, called a T-cell receptor or TCR, that is able to bind to a specific molecular target, like a piece of a virus or bacteria. When a T-cell’s receptor binds to its target, it triggers the cell to go on the attack, launching an inflammatory response to deal with the threat.
In MS, abnormal inflammation in the brain and spinal cord causes damage to the myelin sheath, a fatty coating that covers and protects nerve fibers, helping them to send electrical signals. MS patients frequently have T-cells with receptors that bind to parts of the myelin sheath. These self-targeting T-cells are thought to be centrally involved in driving the disorder.
However, T-cells with receptors that bind to myelin also are found in people who show no sign of MS. This suggests that the presence of these cells alone is insufficient to cause the neurodegenerative disorder.
Other factors must be at play, according to researchers, which in some cases may trigger these cells to go into the brain and launch an inflammatory attack. But what these factors might be has long been a mystery.
In this study, scientists engineered mouse T-cells so they would be equipped with a receptor that binds to myelin oligodendrocyte glycoprotein (MOG), a component of the myelin sheath that’s often targeted by T-cells in MS. The team then injected these cells into mice, and used advanced imaging technology to monitor their movement and activation within the animals’ bodies.
Through these experiments, they found that myelin-targeting T-cells became activated in the ileal lamina propria (LP) — a connective tissue layer in the small intestine.
Researchers then put the myelin-targeting cells into mice that lacked a gut microbiome, which is the community of bacteria and other microorganisms that normally lives in the digestive system. In these mice, myelin-targeting T-cells did not become activated in the ileal LP, demonstrating that their activation in this specific part of the gut depended on the presence of gut microorganisms.
Treating mice with an antibody that blocked MHC class II, a protein that other types of immune cells use to help T-cells recognize their targets, likewise blocked T-cell activation in the ileal LP, the team also found.
These data show “direct evidence to confirm the pivotal role of microbiota in T cell stimulation and highlight the important role of MHC class II,” the researchers wrote.
Findings provide proof of concept for how T-cells become activated
Scientists speculated that myelin-specific T-cells may become activated in the gut because some gut bacteria have proteins that are shaped similarly to myelin, allowing the cells’ receptors to bind to the bacteria and trigger inflammatory activation. But they stressed that further research is needed to test this idea and identify the specific bacteria that may play that role.
The team also found that T-cells with receptors against some non-myelin targets also were activated in the ileal LP, but only in mice with an intact microbiome, suggesting that this phenomenon may not be exclusive to cells that drive MS.
“Interestingly, activation in the lamina propria seems to be a general mechanism, as even for non-[myelin-targeting] T cells, which target other molecules in the body, we found that activation depended on the microbiome,” Kawakami said.
Scientists next conducted studies in which they tracked the movement of T-cells leaving the ileal LP to see where they went next. They found that myelin-targeting cells activated in this part of the gut were then able to migrate into the brain and spinal cord.
At the same time, they started to turn on several genes characteristic of Th17 cells, a specific type of T-cell that’s been heavily implicated in the development of MS.
Taken together, these data provide a proof of concept for how myelin-targeting T-cells might become activated and migrate into the brain, where they would launch an inflammatory attack that ultimately would lead to the development of MS, the team concluded.