Cell-based therapy can be produced in under 3 days from blood sample
KYV-101 is an experimental CAR T-cell therapy by Kyverna Therapeutics
Written by |
Kyverna Therapeutics has developed a method that enables KYV-101, an experimental CAR T-cell therapy for multiple sclerosis (MS) and other conditions, to be produced in a much shorter timeframe than conventional manufacturing processes, a study shows.
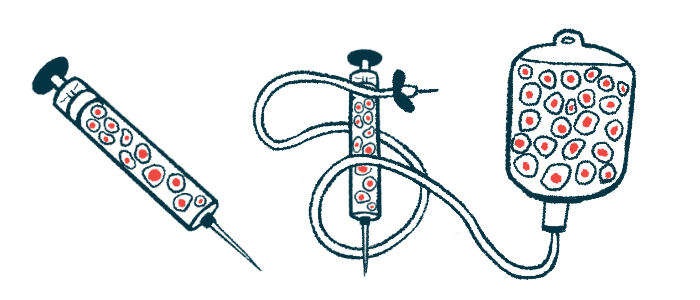
The approach took less than three days to produce KYV-101 from a simple blood draw and the cells were more potent and had more durable activity than the conventionally manufactured product which requires apheresis, a more invasive procedure wherein T-cells are isolated in a machine and grown in a lab until there are millions of them that are then infused back into a patient’s bloodstream.
“We were able to achieve a process minimization without compromising the quality of the operations or the characteristics of the resulting product,” Karen Walker, chief technology officer of Kyverna, said in a company press release.
The study, “Development of Ingenui-T, a Novel Vein-to-Vein Solution for Rapid Autologous CAR T-Cell Manufacturing Starting From Whole Blood, for the Treatment of Autoimmune Diseases,” was published as a preprint in BioRxiv, but hasn’t been peer reviewed yet.
“By eliminating the need for apheresis, we are demonstrating our focus on improving the patient experience, as well as their [caregivers’],” said Peter Maag, PhD, Kyverna’s CEO.
What is KYV-101?
KYV-101 belongs to a class of treatments called CAR T-cell therapies, which involve collecting a person’s immune T-cells and genetically engineering them to carry a special receptor, called a chimeric antigen receptor, or CAR, that recognizes a target.
The receptor in KYV-101 is designed to promote an immune response against antibody-producing B-cells, which factor in autoimmune diseases such as MS and some cancers. It does that by binding to the CD19 protein at their surface.
By eliminating B-cells, or at least dramatically reducing their number, KYV-101 should help control progressive MS. A Phase 2 trial (NCT06138132), due to open soon, will investigate the therapy’s safety and preliminary signs of efficacy in 12 adults with progressive forms of the disease who failed to respond to available medications.
Researchers at Kyverna developed a new approach in collaboration with ElevateBio. Their proprietary platform, Ingenui-T, can produce CAR T-cells from a simple blood draw, yielding about as many cells as conventional methods. Here, the researchers described the process for KYV-101 using less than 200 mL of whole blood from nine healthy donors.
After being collected, the blood was mixed with tiny magnetic beads with a special coating that lets them stick to T-cells, enabling researchers to easily separate these cells from the remaining blood components.
These isolated cells were genetically engineered to produce a CD19 CAR receptor and remained in culture for less than three days to recover and integrate the CAR gene into their genome. They were then harvested, washed, and prepared for intravenous (into-the-vein) infusion into healthy donors.
“Starting from a whole blood draw instead of apheresis, combined with a shorter duration of CAR T-cell manufacturing, holds the potential to revolutionize the patient experience of CAR T-cell therapy,” the researchers wrote.
A better yield
Using this approach, 93.9% of the final product were T-cells. These T-cells came from an initial batch of whole blood where they made up 42.3% of the total cells. Conventional apheresis yielded 94% of T-cells from an initial batch of 46.3%.
Despite a short manufacturing time, the Ingenui-T approach yielded 38.5 millions of T-cells per 100 mL of whole blood. About half were CAR T-cells, similar to the proportion obtained using conventional methods.
When grown in the lab together with immune B-cells, CAR T-cells prepared with Ingenui-T destroyed B-cells more effectively than conventional CAR T-cells at the same dose.
The Ingenui-T product also was richer in younger, less differentiated (specialized) T-cells, “with potentially improved clinical benefit.” Growing cells in the lab for prolonged periods before infusion may result in more mature and older cells, which are more likely to become exhausted and be less effective.
“These results have paved the way for the clinical development of Ingenui-T cells,” the researchers wrote, adding the T-cells “will improve the patient experience, increase treatment accessibility, and reduce costs, by eliminating the need for patients to undergo apheresis.”