Small molecule promotes myelin sheath repair in MS mice: Study
Mice saw improved motor function, nerve cell communication
Written by |
A small molecule called ESI1 stimulated the repair of the myelin sheath, the fatty coating on nerve fibers that is damaged in multiple sclerosis (MS), a study found.
In an MS mouse model, this resulted in improved motor function and nerve cell communication, as well as reduced signs of disease-driving inflammation. ESI1 also enhanced myelin repair in aged healthy mice while reversing cognitive decline.
“Currently, there are no effective therapies to reverse myelin damage in devastating demyelinating diseases such as MS,” lead author Q. Richard Lu, PhD, scientific director at the Cincinnati Children’s Hospital Medical Center’s Brain Tumor Center, said in a hospital press release. “These findings are significant as they offer new pathways for treatment that potentially shift the therapeutic focus from just managing symptoms to actively promoting repair and regeneration of myelin.”
The study, “Small-molecule-induced epigenetic rejuvenation promotes SREBP condensation and overcomes barriers to CNS myelin regeneration,” was published in the journal Cell.
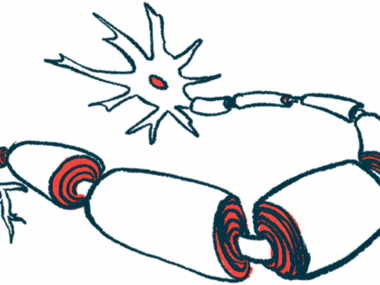
The myelin sheath is a fatty protective layer that forms around nerve fibers in the central nervous system (CNS), which comprises the brain and spinal cord. Produced by neighboring cells called oligodendrocytes, it helps to speed up the transmission of electrical impulses along nerve fibers. In MS, immune-mediated damage to the myelin sheath (demyelination) impairs nerve function and communication, which gives rise to MS symptoms.
Understanding barriers to myelin sheath repair
Evidence suggests that, in areas of myelin damage, the ability of oligodendrocytes to repair the myelin sheath (remyelination) is impaired. Although defects in the growth of oligodendrocyte precursor cells were thought to be the cause, recent data indicate that mature cells also fail to properly remyelinate nerve fibers in MS lesions.
“The molecular barriers that prevent [oligodendrocytes] from producing myelin are poorly understood, and no effective treatments are available that reverse myelin damage or promote remyelination,” Lu and his colleagues wrote.
To better understand those barriers, the team first examined oligodendrocyte function in post-mortem tissue samples from MS patients with both active and inactive demyelinated lesions. While levels of mature oligodendrocytes in MS lesions were comparable to healthy brain regions, the cells inside lesions were epigenetically silenced.
Epigenetics refers to cellular processes that control the activation or deactivation of gene expression without altering a gene’s DNA sequence. Here, epigenetic silencing, or suppression of gene activity, was found to be the barrier that prevented oligodendrocytes from remyelinating nerve fibers in MS lesions.
After screening a library of compounds to find those that block enzymes involved in epigenetic silencing, ESI1 (epigenetic-silencing-inhibitor-1) was identified as the most potent, boosting myelin production by about five times compared with the second-strongest compound.
When demyelination was induced in mice, ESI1 promoted remyelination and increased myelin thickness when the myelin repair processes had already begun. ESI1 also enabled the production of new myelin on regenerated nerve fibers following induced nerve damage.
ESI1 was then evaluated in a well-characterized MS mouse model called experimental autoimmune encephalomyelitis, or EAE, which, like in MS patients, has immune-mediated damage to the myelin sheath. Without treatment, EAE mice developed chronic hindlimb paralysis, but disease severity was markedly lower in ESI1-treated EAE mice.
In the lower spinal cord, the area most affected in EAE mice, ESI1-treated animals showed more signs of remyelination and less inflammation than controls, “suggesting that ESI1 may have an immunomodulatory activity,” the researchers wrote.
In line with these findings, ESI1 significantly improved motor function and nerve cell communication in EAE mice.
ESI1 also boosted myelination in healthy-aged mice, slowed age-related cognitive decline, and stimulated remyelination following demyelinating injury.
To explore ES1’s potential effectiveness in MS patients, the team tested ESI1 in lab-grown brain organoids, which contain cells arranged in a three-dimensional architecture that resembles the human nervous system. Here, ESI1 promoted the activity of genes associated with myelin generation and stimulated myelin sheath extension.
Mechanism-of-action experiments demonstrated that ESI1 triggered remyelination by blocking the activity of an enzyme called HDAC3, a known epigenetic suppressor of gene expression.
But independent of HDAC3 inhibition, the compound also exerted its function by activating SREBP1a and SREBP2, proteins that drive the production of fatty acids and cholesterol in oligodendrocytes, the main components of the fatty myelin sheath. “Our study highlights the potential of targeting epigenetic silencing to enable CNS myelin regeneration in demyelinating diseases and aging,” the researchers wrote.
“This study is a beginning,” Lu said. “Prior to finding ESI1, most scientists believed that remyelination failure in MS was due to the stalled development of precursors. Now we show a proof of concept that reversing the silencing activity in [oligodendrocytes] present in the damaged brain can enable myelin regeneration.”