$2.9M research grant funds technology for MS stem cell therapy
University at Buffalo scientists win funding for injection research
Written by |

The National Institute of Neurological Disorders and Stroke has awarded a $2.9 million, five-year grant to a research project that aims to advance a new technology that could improve stem cell therapies for multiple sclerosis (MS) and other neurological disorders.
“The work we plan to undertake has significant implications for regenerative medicine, as it has the potential to develop novel strategies to enhance stem cell delivery for treatment of devastating neurological diseases that remain intractable to current treatments,” Stelios Andreadis, PhD, director of the University at Buffalo’s Cell, Gene and Tissue Engineering Center and one of the project’s leaders, said in a university press release.
Fraser Sim, PhD, a professor at the university’s Jacobs School of Medicine and Biomedical Sciences and the director of its neuroscience program, will co-lead the project. “This project is a wonderful example of collaborative science,” Sim said. “Neither of us could do this work alone.”
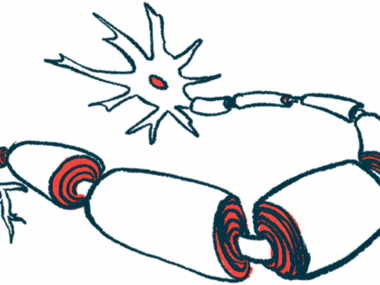
In MS, inflammation in the brain and spinal cord causes damage to myelin, a fatty substance that wraps around nerve fibers and helps them send electrical signals. Myelin damage disrupts neurological signaling, which ultimately gives rise to MS symptoms.
Stem cell therapies for MS and other neurological disorders are gaining increasing interest from researchers. Stem cells are a special class of cells that are able to grow into other types of cells.
Designing hydrogels to protect cells during injection
The basic aim of stem cell therapy in MS is to introduce stem cells that could make new nervous system cells, such as neurons (nerve cells) and myelin-making cells like oligodendrocyes and Schwann cells.
In order to be used as a therapy, the stem cells need to be injected into a patient’s brain. In experiments, this has usually been done by simply suspending the cells in a saline solution and injecting them through a syringe.
But emerging data suggest that the physical stress of being suspended in liquid and then squeezed through the needle tends to damage the cells, and as a result, the vast majority of stem cells end up dying soon after they are injected.
Most researchers have “just accepted the fact that a lot of cells will die when you transplant them,” Sim said. The new project aims to change this.
The researchers are working to develop shear-thinning hydrogels (STHs) to aid in stem cell injections. STHs normally have a gel-like consistency, but become more fluid when pressure is applied — for example, when squeezed through a syringe. The general idea is that STHs can help cushion and protect stem cells during injection.
“They change their viscosity in response to shear stress, and they can turn back into gel form when the force is removed, after the injection,” Andreadis said. “The fast transition from solid-like to fluid-like behavior, with increasing shear rate, is essential for successful injection and cell protection.” STHs “have emerged as promising candidates for the injection of Schwann cells and oligodendrocytes,” he said.
Mouse experiments showed improved cell survival with STHs
In addition to cushioning the cells, the STHs can also be tailored to help promote the cell’s survival once inside the brain.
“With the hydrogel, we can introduce different factors that will allow the cells to overcome the [suppressive] environment that’s present in MS lesions,” Sim said. “We think this will improve the outcome of cell therapy over the vanilla approach using cells in a saline solution.”
The researchers have already conducted proof-of-principle experiments of STHs in mice genetically engineered to be unable to make myelin, mimicking a rare progressive neurodegenerative condition called Pelizaeus-Merzbacher disease.
Transplanting human cells with STHs into the animals’ brains “significantly improved the survival of the transplanted cells and enhanced nerve repair in the brain 12 weeks post-implantation,” Andreadis said.
Those results will be published in full soon, the university said.
In the newly funded project, the researchers will test STHs in larger animals, aiming to determine the number of cells needed for a brain that’s closer in size to a human brain and assess whether the cells are going to the intended parts of the brain.
“This is a great opportunity to marry biomaterials science and engineering with neuroscience to develop a therapeutic strategy that can, hopefully, be brought to the clinic to treat devastating diseases and conditions such as MS,” Andreadis said. “While there is currently no cure, we would like to develop a successful therapy that can limit the disease’s development and improve quality of life for MS patients and others who are suffering from neurological disorders.”