
Symptoms of secondary progressive MS
Last updated Oct. 20, 2025, by Lindsey Shapiro, PhD

The symptoms of secondary progressive multiple sclerosis (SPMS) are similar to those seen in other forms of multiple sclerosis (MS), but they tend to be more severe and gradually worsen over time.
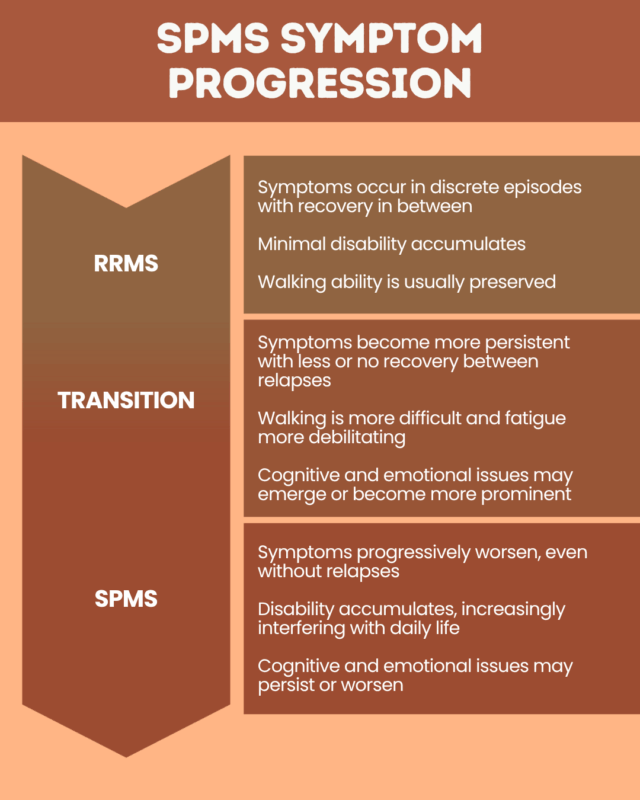
In MS, the immune system mistakenly attacks healthy tissue in the brain and spinal cord. Most people are first diagnosed with relapsing-remitting MS (RRMS), which is characterized by episodes of new or worsening symptoms, called relapses, followed by periods of remission when symptoms ease or disappear.
SPMS is a type of MS that develops after an initial relapsing-remitting phase. It represents a stage in which the disease progresses more steadily, with symptoms that persist and get gradually worse over time, even in the absence of relapses.
It is important for people with MS to monitor changes in their symptoms carefully, as neurologists use this information to determine when a person has transitioned from RRMS to SPMS and whether changes to their treatment plan are needed.
Common physical symptoms
In SPMS, accumulating damage in the brain and spinal cord causes a gradual decline in physical function. While the common physical symptoms of SPMS are similar to those seen in RRMS, they tend to be more persistent and progressive, often having a greater impact on daily life and leading to worsening disability over time.
There is no single course of progression in SPMS, so the exact symptoms and how quickly they worsen can vary from person to person. Still, some of the most common SPMS symptoms include:
- difficulty with walking and balance
- gradually worsening muscle weakness, stiffness, or spasticity
- sensory changes such as pain and numbness, tingling, or itching sensations
- profound and persistent MS fatigue
- bladder and bowel problems, including loss of bladder control and constipation
- vision problems
Mobility issues in SPMS are more common than in RRMS and may lead to an increasing need for mobility aids such as canes or wheelchairs. For some people, trouble walking may be one of the first signs they have transitioned from RRMS to SPMS.
The physical symptoms of SPMS are similar overall to those of primary progressive MS (PPMS), where MS symptom progression occurs from the onset of the disease.
People with SPMS may still experience relapses, but recovery is often less complete than in RRMS, and periods of full remission become less frequent or nonexistent.
Less common symptoms
Various other symptoms are also possible with SPMS progression. These include:
- speech and swallowing difficulties
- tremors, or uncontrolled shaking
- breathing problems
- hearing or taste loss
- seizures
The exact symptoms a person with SPMS experiences can vary based on which parts of the brain or spinal cord are most affected.
Cognitive and emotional symptoms
MS cognitive changes tend to be more frequent in SPMS than in RRMS, often worsening as the disease advances and significantly affecting daily life.
Cognitive symptoms in MS may include:
- difficulties with memory and concentration, such as forgetting appointments or struggling to stay focused on a task
- slower processing speeds, meaning it takes longer to absorb, process, and respond to information
- impairments in executive function, the higher-level skills needed to plan, organize, problem solve, and make decisions, which can make it harder to manage daily responsibilities
Many people with SPMS also experience mental health issues and MS mood changes, which may stem from both neurological damage and the stress of living with a chronic, progressive condition. These can include:
- depression or anxiety
- feelings of grief, frustration, or anger
- mood swings
- pseudobulbar affect, a neurological syndrome characterized by sudden, uncontrollable episodes of crying or laughing, often out of proportion or unrelated to actual emotions.
Recognizing symptom progression
The pace of transition from RRMS to SPMS can vary. For some people, changes in symptoms occur so gradually that they may be hard to notice at first, while for others, this shift is more sudden and apparent.
After a diagnosis, it’s important for people with MS to regularly track their symptoms — for example, by keeping a diary or using a symptom-tracking app — and to inform their healthcare team if symptoms become more frequent or persistent. Some changes that may suggest a progression toward SPMS include:
- feeling unable to walk as fast or as far as before, falling more often, or relying more on walking aids
- worsening muscle stiffness or spasticity that makes everyday tasks more difficult
- feeling the need to use the bathroom more urgently or frequently, or having accidents
- fatigue that is more constant or increasingly interferes with daily activities
- difficulty concentrating, worsening forgetfulness, or other cognitive challenges that feel more persistent
Any symptoms that don’t improve between relapses, or that are getting progressively worse over time, could indicate a transition from RRMS to SPMS.
It is important to notify a doctor about any noticeable changes in MS symptoms. Identifying progression as early as possible allows healthcare providers to adjust treatment strategies for better managing MS symptoms and make living with SPMS easier.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recommended Posts
- Long-term air pollution exposure may increase risk of developing MS: Study
- The silent grief I carry beneath the surface with MS
- Guest Voice: Navigating the uncharted path of living a full life with MS
- New CSF protein markers may help support multiple sclerosis diagnosis
- Caring for others while living with MS requires finding balance




