FAQs about Tysabri in MS
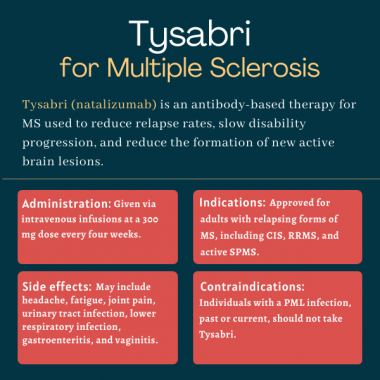
Tysabri was approved in the U.S. in November 2004 to treat relapsing forms of multiple sclerosis — including clinically isolated syndrome, relapsing-remitting MS, and active secondary progressive MS. The U.S. Food and Drug Administration also approved Tysabri for patients with Crohn’s disease, a form of inflammatory bowel disease, in 2008.
According to Biogen, Tysabri begins to demonstrably reduce the risk of relapse as soon as two months after starting the therapy. Nonetheless, every person with MS is unique, and patients are advised to discuss with their healthcare team how the medication may help in their specific case.
Based on animal data, Tysabri may cause harm to a developing fetus. Therefore, the medication should only be used during pregnancy if the potential benefits of treatment justify the potential risk to the unborn child. Those who become or plan to become pregnant while on Tysabri should discuss the potential benefits and risks with their healthcare providers as early as possible.
Tysabri is not known to interact with alcohol. Nonetheless, since alcohol can interfere with some medications and worsen certain MS symptoms, patients should discuss safe alcohol consumption with their healthcare provider.
It is possible that patients on Tysabri may experience changes in body weight. In a clinical trial called AFFIRM, about 2% of patients given Tysabri experienced an increase in body weight, and a similar percentage had a decrease in body weight. Hair loss, however, was not reported as a side effect of Tysabri in clinical trials. Patients who experience any unexpected weight changes or unexplained hair loss should talk to their healthcare providers.
Related Articles

 Fact-checked by
Fact-checked by