Vitamin D and multiple sclerosis
The relationship between vitamin D and multiple sclerosis (MS) is relatively well established. Low vitamin D levels, or vitamin D deficiency, are considered an environmental factor that increases MS risk and may also contribute to worse disease outcomes.
Vitamin D helps regulate the immune system, which may partly explain its connection to autoimmunity in MS. Still, researchers are continuing to study how vitamin D levels affect disease activity and progression after an MS diagnosis and whether vitamin D supplementation in MS offers meaningful benefits.
What is vitamin D?
Vitamin D supports many functions in the body, helping with calcium absorption and bone strength, supporting brain and muscle health, and reducing inflammation.
It can be obtained from dietary sources and is directly produced in the skin after exposure to sunlight. Vitamin D exists in two primary forms:
- vitamin D3 (cholecalciferol), obtained from sunlight exposure and animal-based dietary sources
- vitamin D2 (ergocalcigerol), obtained from plants and fungi
Both forms are inactive. The liver first converts them into an intermediate molecule called 25-hydroxyvitamin D (25[OH]D), also called calcidiol. The kidneys then convert that into the active form, 1,25-dihydroxyvitamin D (1,25[OH]2D), or calcitriol.
Active vitamin D works by binding to vitamin D receptor proteins found in cells throughout the body. This complex then interacts with DNA to help regulate which genes are turned on or off.
How does vitamin D affect MS?
Vitamin D may affect MS in several biological ways. It is considered a potent immune modulator, helping regulate the activity of B-cells, T-cells, and other immune cells implicated in MS.
Some preclinical studies suggest vitamin D may play a direct role in repairing myelin, a protective sheath around nerve fibers that is damaged in MS, although evidence in humans is still limited.
Vitamin D and MS risk
Scientists have studied the relationship between vitamin D and MS for decades, and evidence supports a link between vitamin D deficiency and MS risk:
- People with low vitamin D blood levels are consistently more likely to develop MS than those with normal levels.
- MS risk during adulthood is much higher in people exposed to low vitamin D levels in utero or who had low levels of the vitamin in infancy.
- Lower exposure to sunlight — the main source of vitamin D — is strongly associated with higher MS risk, with MS being more common in regions farther from the equator.
- People with genetic alterations that result in lower vitamin D levels have a higher susceptibility to MS.
- People who obtain less vitamin D from supplements or food have a higher incidence of the disease.
Vitamin D and MS outcomes
While the link between vitamin D and MS risk is clear, its impact on MS outcomes is less certain.
Some studies suggest that people with lower vitamin D levels experience more frequent relapses and faster disability progression, and that supplements may reduce disease activity. However, clinical trials testing high-dose vitamin D supplementation have shown mixed or inconsistent results:
- A Phase 3 trial called D-Lay MS (NCT01817166) found that high-dose vitamin D (100,000 international units, or IU, every other week) significantly reduced the risk of new disease activity on MRI scans in people with clinically isolated syndrome or early relapsing-remitting MS (RRMS), but no significant differences were observed for MS relapse rates or disability progression.
- A Phase 3 trial called VIDAMS (NCT01490502) found that high-dose vitamin D (5,000 IU/day) did not significantly lower the risk of relapse relative to low-dose vitamin D (600 IU/day) among RRMS patients.
- The Phase 2 SOLAR clinical trial (NCT01285401) found that high-dose vitamin D (14,007 IU/day) did not reduce the rate of relapses or disability progression among RRMS patients, although it did reduce the development of brain lesions.
- The Phase 2 CHOLINE trial (NCT01198132) found that high-dose vitamin D3 (100,000 IU every other week) did not significantly lower relapse rates in the overall population of RRMS patients, but other analyses suggested a clinical benefit in relapse rates, MRI activity, and MS disability progression among participants who completed the full study.
How to test vitamin D levels
While the active form of vitamin D is calcitriol, vitamin D status is assessed using a blood test that measures its precursor molecule, 25(OH)D. This is the best indicator of vitamin D availability in the body.
Optimal vitamin D
There is no universal consensus on the optimal vitamin D level in MS or the general population. However, most guidelines define 25(OH)D levels below 20 nanograms (ng)/mL as vitamin D deficiency.
Levels above 20-30 ng/mL may be sufficient for most people, although some experts suggest higher values are ideal. The 2024 Endocrine Society guidelines indicate more research is needed to determine optimal levels.
Currently, there are no specific vitamin D supplementation guidelines for MS. A person’s doctor will determine when assessing vitamin D status in MS patients is appropriate, and whether low 25[OH]D levels in MS should be treated with supplementation.
Vitamin D sources
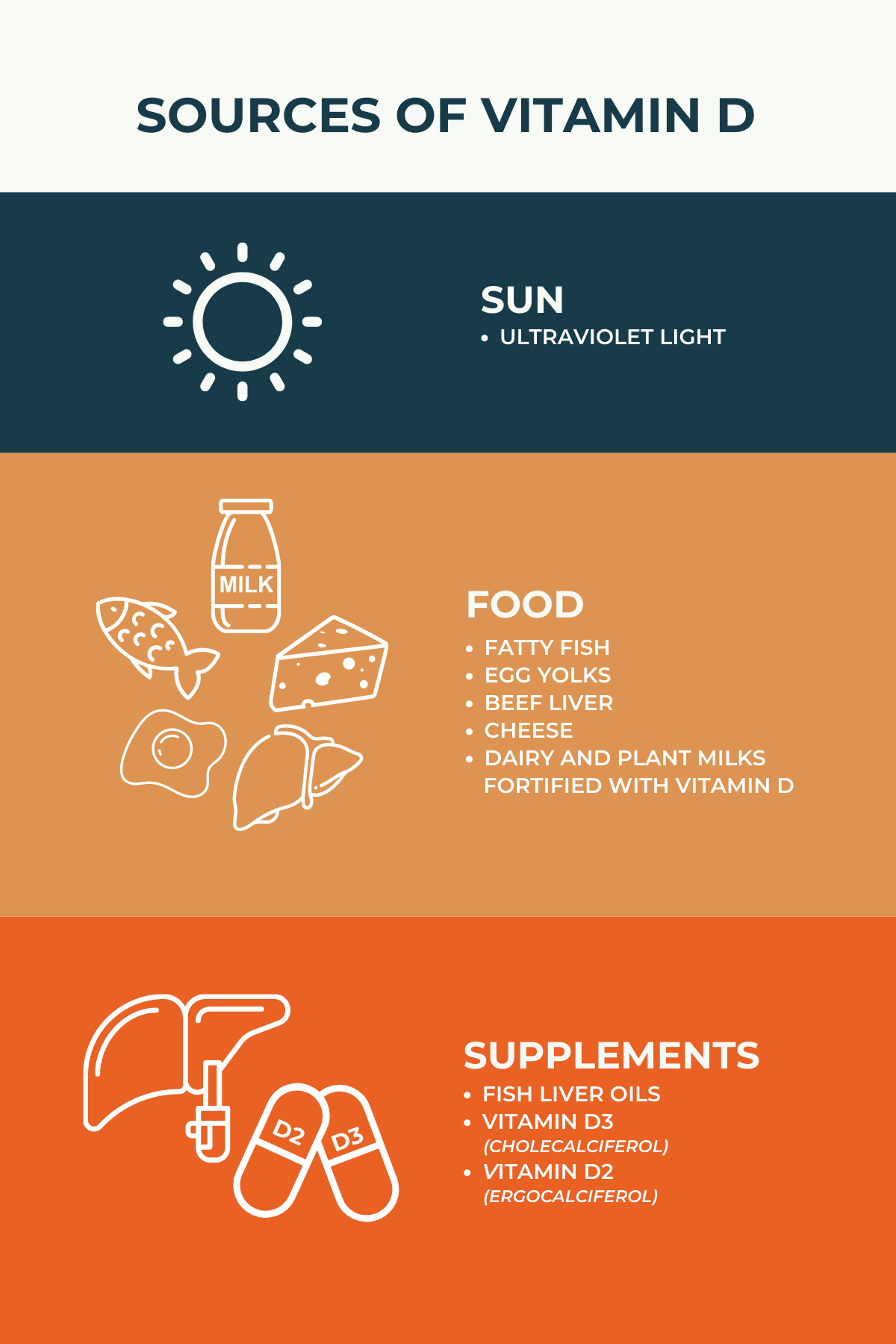
The body obtains vitamin D from three main sources:
- Sunlight: Most vitamin D comes from sunlight, specifically ultraviolet B light exposure. How much vitamin D a person produces from sunlight depends on several factors, including skin color, age, sunscreen use, season, and geographical location.
- Food: Vitamin D can also be obtained through diet, although to a lesser degree. Natural sources include fatty fish, egg yolks, beef liver, and mushrooms. Many cereals, dairy products, and juices are also fortified with vitamin D.
- Supplements: Dietary supplements are another source of vitamin D and may include fish liver oils or pills containing vitamin D2 or vitamin D3. Healthcare providers determine the appropriate dose and schedule based on a person’s health needs.
Can you take too much vitamin D?
Vitamin D toxicity is rare but possible, usually from taking too many supplements. Extremely high vitamin D levels, typically above 150 ng/mL, can cause dangerously high calcium levels in the blood.
Symptoms of very high vitamin D may include:
- digestive problems such as vomiting, nausea, or constipation
- excessive urination
- dehydration and excessive thirst
- muscle weakness
- confusion, irritability, or fatigue
- kidney complications
- heart problems
Vitamin D toxicity is unlikely to occur from sun exposure or diet but may develop after taking high-dose vitamin D supplements. To prevent complications, people should follow medical guidance and avoid taking high-dose supplements unless supervised by a healthcare provider.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by 

