Specific Gut Bacteria May Drive Progression of Multiple Sclerosis, Study Finds
Written by |
Specific gut bacteria may drive the progression of multiple sclerosis, according to a study showing that two bacterial species made the disease worse in a mouse model of MS.
Researchers at the University of California, San Francisco also pinpointed a species — found in lower numbers in MS patients — that had protective properties in mice with the condition. This demonstrated the power that gut microbes have over the immune system in MS.
The study could be the first step toward therapies that target these gut inhabitants as a way of obtaining control over the disease.
Researchers published the study, “Gut bacteria from multiple sclerosis patients modulate human T cells and exacerbate symptoms in mouse models,” in the journal PNAS,
Our closest environmental link
What prompted researchers to look at the microbiome was the knowledge that genetics play a relatively small part in the risk of someone developing MS.
“The field has been very successful in identifying genes associated with susceptibility to MS, but I’ve never been satisfied with amount of risk that we’ll be able to explain with just genetics,” Sergio Baranzini, a neurology professor who was the senior investigator of the study, said in a university news release.
“Even identical twins, who share the same genetic inheritance, only share an MS diagnosis about 35 percent of the time,” he said. “It’s clear the genome is important, but environmental factors must also play a major role.”
Another clue to the role of environmental factors is a surge in autoimmune diseases, including MS, in the past century, researchers said.
But environmental factors are often difficult to associate with a condition. Yet, research in the past decade has made it clear that our gut is directly linked to the actions of the immune system. This close connection prompted researchers to look at whether clues to MS could be found in the gut.
In 2014, they started delving in to the role of bacteria in MS.
“This was such a novel question, especially at that time,” said Egle Cekanaviciute, a postdoctoral researcher on the team and first author of the study. “No one had looked at the microbiome in MS. Almost no one had looked at the role of gut microbes beyond digestive diseases.”
To start the investigation, the team recruited 71 relapsing-remitting MS patients and as many healthy controls.
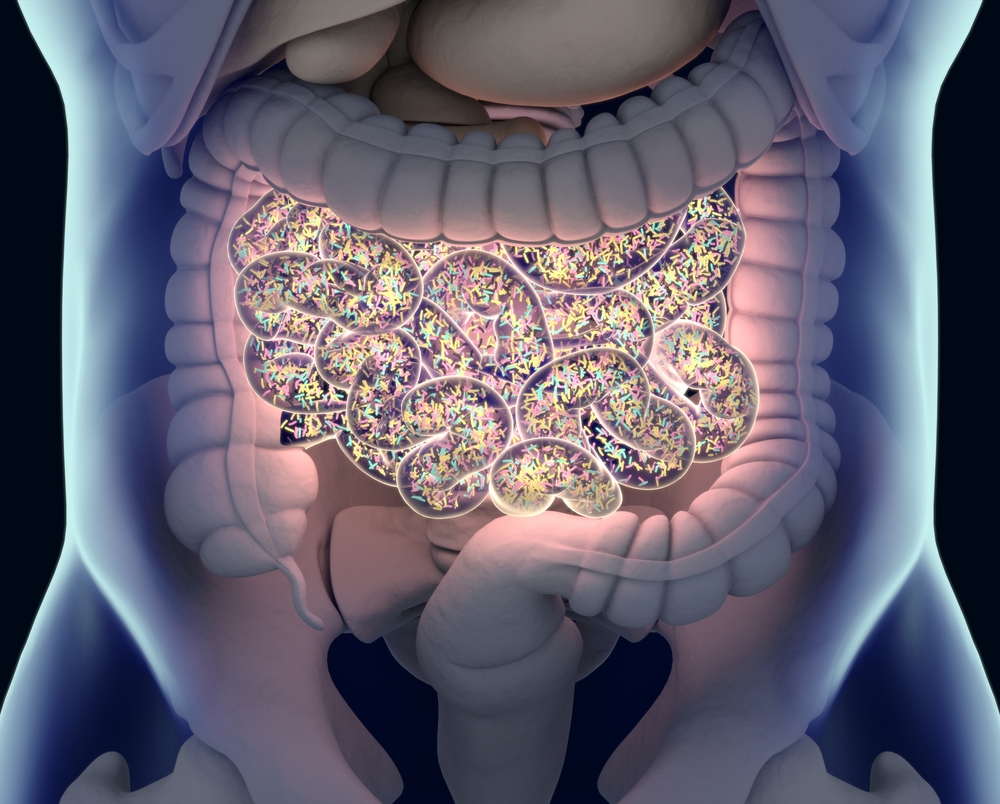
They analyzed their gut microbiome — the entire collection of bacteria residing in the intestines. While they did not find any differences between patients and controls when looking at groups and families of bacteria, they did identify two species that were more common in MS and one that was less common.
Looking for relevance
“A lot of microbiome studies say, ‘These bacteria are increased in patients with a disease, and those bacteria are reduced.’ And then they stop,” Cekanaviciute said. “We wanted to know more. Should we care about the ones that are increased because they are harmful, or the ones that are decreased because perhaps they are helpful? What do these microbes actually do that could have an impact on people’s health?”
To answer these questions, the team first exposed human immune cells, grown in a lab, to components of the bacteria, using a crude bacterial extract.
It turned out that the two species found in higher numbers in patients — Akkermansia (A.) muciniphila and Acinetobacter (A.) calcoaceticus — increased inflammatory in the lab-grown cells.
The species that was reduced in patients, Parabacteroides (P.) distasonis, stepped up protective regulatory immune actions.
Researchers then separately introduced each of these bacteria into mice that had been raised with a microbe-free gut. This would allow each species to dominate the animal’s gut flora.
The mice reacted in much the same way the cells did in the previous experiment. The bacteria that were more common in MS triggered an inflammatory response in the animals, and the one that was reduced hampered inflammation by boosting regulatory T-cells, or Tregs.
Twice the evidence
Since one dominant species is not a typical scenario in humans, the team also wanted to examine how the bacteria would influence an animal with an intact gut flora.
One of their experiments involved transplanting fecal matter from humans to mice. They use three MS patients and three paired controls from the same households. The transplants demonstrated that the bacteria had the power to influence disease.
Mice that had MS fecal transplants developed a more severe disease and had lower numbers of helpful Tregs in their blood. This finding suggested that gut bacteria alone have the power to influence disease progression in MS.
Interestingly, this was not the only study coming to the same conclusion. Cekanaviciute and Baranzini also contributed to a study at the Max Planck Institute in Germany. There, researchers used a different mouse model of MS with the same fecal transplant approach, and got the same results.
“Two different groups, using two separate cohorts of patients and controls, and two distinct mouse models of the disease, saw very similar results. This is very promising evidence that we’re on the right track,” Cekanaviciute said.
New treatments
The researchers hope other scientists pick up their findings to better understand if, and how, the bacteria contribute to MS.
“To be clear, we don’t think the microbiome is the only trigger of MS,” Cekanaviciute said. “But it looks like these microbes could be making the disease progression worse or better — pushing someone with genetic predisposition across the threshold into disease or keeping them safe.”
Other environmental factors likely play a part in the development and progression of the disease as well, researchers said.
So far, the team has found some clues to what might be going on. One of the bacteria found in higher numbers in MS patients produces proteins similar to those found in myelin. Researchers think that the immune system could confuse the factors to attack myelin in addition to the bacteria. Scientists say deterioration of the myelin shield that protects neurons is the cause of MS.
Researchers also think that the bacterial species found in lower numbers in MS help prevent the immune system from attacking harmless gut microbes. Without these helpful species, the immune system might overreact to gut bacteria.
Further insights could lead to new ways of treating MS, researchers believe.
“The microbiome is very malleable,” they wrote. “You could relatively easily change it in an adult who has MS or is susceptible — something you cannot do with their genetics. This is not a magical approach, but it is hopeful.”


