#EAN2018 – Both Brain and Spinal MRIs Needed to Monitor MS Inflammation, Study Says
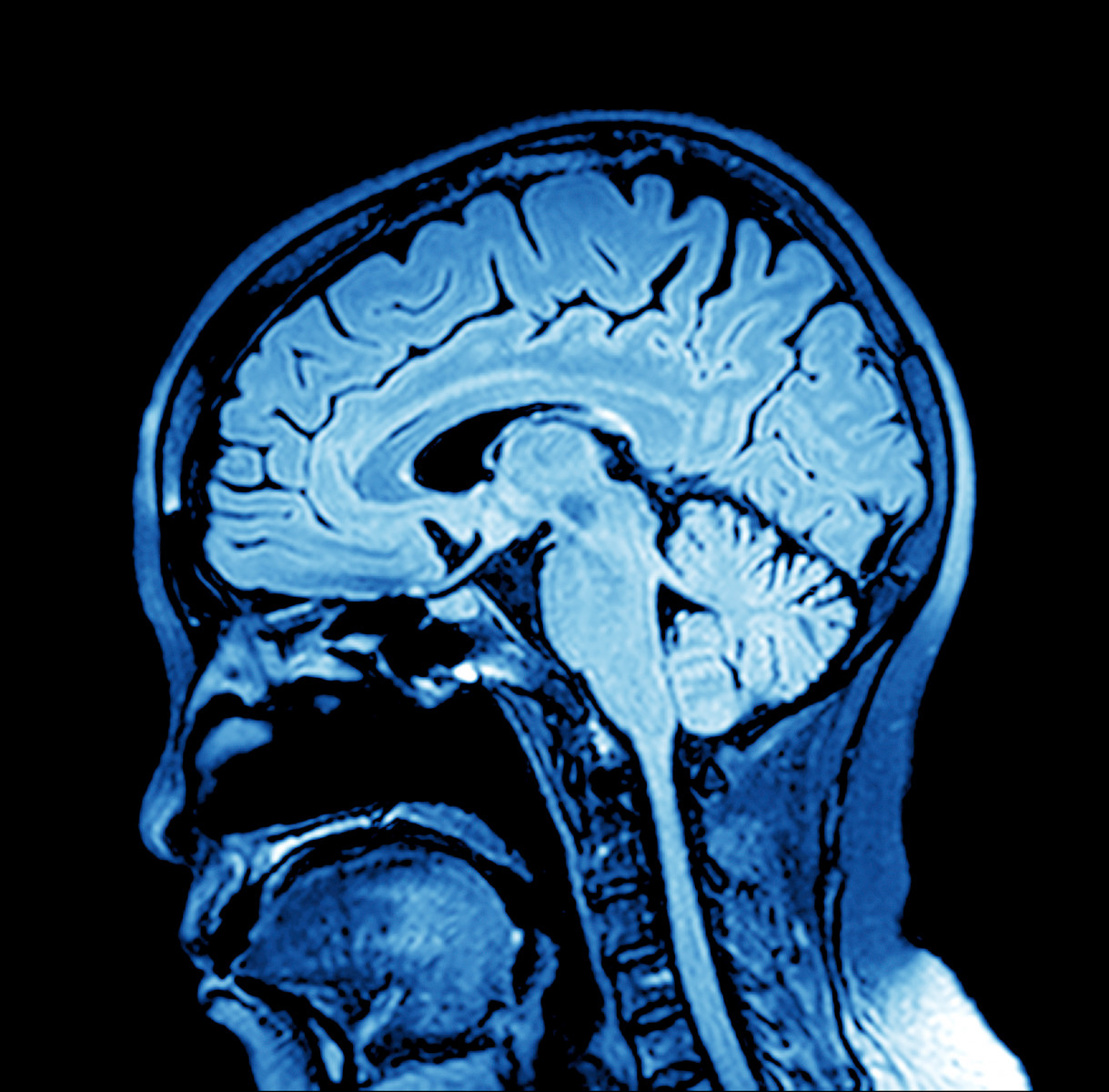
Magnetic resonance imaging (MRI) used to assess inflammation in multiple sclerosis (MS) patients should include scans of the spinal cord and not be restricted to the brain, because brain scans alone risk underestimating disease progression, a study suggests.
These results were shared in the presentation, “Measuring disease activity in Multiple Sclerosis: do we need spinal cord MRI?” (abstract on page 71) given at the 4th Congress of the European Academy of Neurology (EAN) that recently concluded in Lisbon.
When MS is suspected in a person, guidelines recommend an MRI of the spinal cord and brain to reach a diagnosis. But to monitor disease progression in people with confirmed MS, only brain MRIs are typically taken.
Whether spinal MRIs are also effective at monitoring progression is still controversial.
The researchers hypothesized that “using brain MRI only might fail in detecting inflammation in a proportion of patients.”
They investigated the frequency of spinal cord acute inflammation, and whether this occurred independently from brain activity. Their study looked at data on MS patients who underwent at least two different MRIs (brain and spinal cord) at least 30 days apart, and had MRI reports available.
Join our FORUMS to discuss the latest research and trials!
Inflammatory activity was defined by the presence of at least one gadolinium-enhancing lesion according to its location (either in the brain, the spinal cord, or both). Gadolinium (Gd), also called a “contrast” agent, is a harmless chemical compound given by injection that passes from a patient’s bloodstream to sites of active inflammation in the brain or spinal cord where it lights up, creating a visual image on an MRI that flags an inflammation site.
The team analyzed 5,717 scans, of which 4,537 (79.3%) showed no Gd enhancement.
Out of the remaining 1,180 scans, 651 (55.2%) showed brains with only Gd-enhanced lesions, and 232 (19.7%) had Gd-enhanced lesions in both the brain and spinal cord.
However, 297 (25.2%) of these scans showed Gd-enhanced lesions only in the spinal cord.
Disease-induced spinal cord damage can occur independently of damage taking place in the brain, the study concluded.
“Our study demonstrates that inflammatory activity can be detected frequently in SC [spinal cord] and occurs in approximately 25% alone. Limiting MRI monitoring to brain, underestimates inflammatory activity,” the researchers wrote.
“MRI monitoring of SC [spinal cord] in clinical practice will allow neurologists to switch treatment to more powerful drugs” as needed, the team added.