Phagocytes, Key Immune Cells, Seen to Switch from Promoting to Repairing MS Lesions in Study
Written by |
Phagocytes, diverse cells of the innate immune system, are known to both promote and prevent inflammation, depending on whether they are programed to damage tissue or to repair it. A study in mouse model of multiple sclerosis (MS) now reports that this programming is not fixed, and that pro-inflammatory phagocytes found in abundance around lesions in patients can switch states and turn protective.
Earlier MS research had suggested two different types of phagocytes — one good, one bad — might be at work in the central nervous of MS patients, implying a fixed phenotype (or characteristics) for these cells. This study, by scientists in Germany, suggests these immune cells are greatly influenced by the “local microenvironment” and can be adaptive, with implications for how they are targeted by MS treatments.
The research, “Mononuclear phagocytes locally specify and adapt their phenotype in a multiple sclerosis model,” was published in the journal Nature Neuroscience.
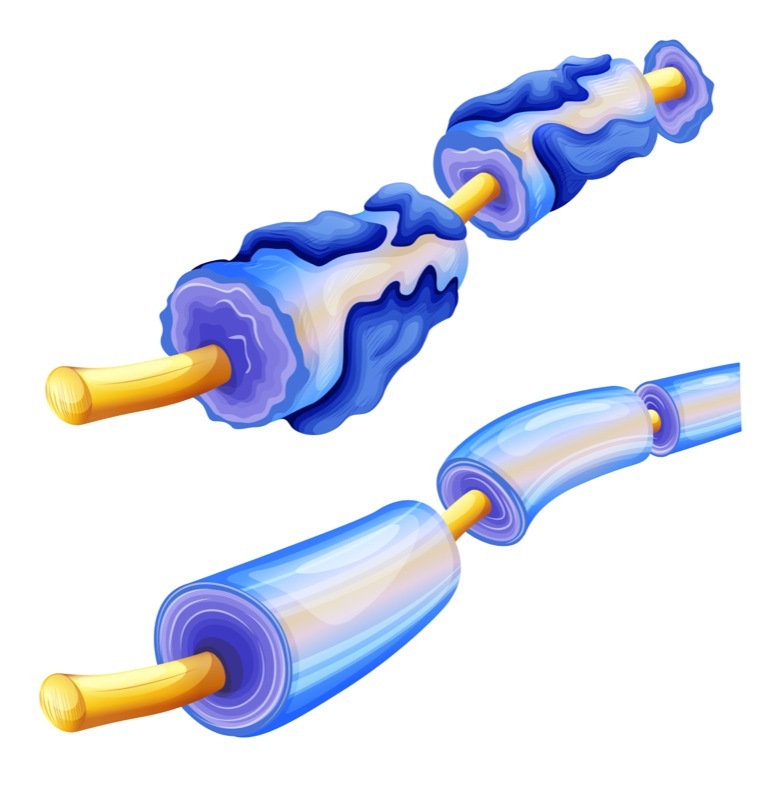
Mononuclear phagocytes are an important and specialized group of cells of the innate immune system, the body’s first line of defense against pathogens. They include microglia, monocytes, macrophages, and dendritic cells — all working to engulf, digest and expel harmful invaders, like microbes, or damaged cells.
Although phagocytes are key to protecting the body from damage and repair injuries, they also are prime players in the development of inflammatory diseases of the central nervous system (spinal cord and brain), including MS.
Microglia and macrophages are the dominant cell types found in MS lesions, and their presence is associated with damage to nerve fibers (axons) and the loss of the protective myelin sheath that coats them.
The dual nature of these in the CNS has continued to puzzle researchers.
Interested in MS research? Sign up for our forums and join the conversation!
Scientists at Ludwig-Maximilians University Munich investigated the behavior of mononuclear phagocytes in the spinal cord of an established MS mouse model, called experimental autoimmune encephalomyelitis (EAE).
Using a fluorescent tracking system capable of marking single phagocyte cells, they followed the behavior and actions of individual phagocytes continuously, and in real time, under a microscope.
They observed that the functional properties of phagocytes were not fixed — rather, they shifted throughout the process of lesion formation and resolution.
“We show that the initial proinflammatory polarization of phagocytes is established after spinal cord entry and critically depends on the compartment they enter,” researchers wrote.
Then, as lesions evolve to remission, individual phagocytes switch their behavior toward one that works to inhibit inflammation and promote repair. This switch appears to be guided by signals released by different CNS environments.
“In subsequent experiments, we demonstrated that this phenotypic conversion is induced by signals from the central nervous system, in particular by soluble factors secreted by cells known as astrocytes [cells that provide support, nutrients and help repair nervous tissue],” Martin Kerschensteiner, director of the Institute of Clinical Neuroimmunology at LMU and the study’s senior author, said in a press release.
“[O]ur findings are consistent with the existence of a rather continuous spectrum of phagocyte phenotypes, along which phagocytes can move depending on cues they received from the lesion environment,” the study states.
Together, these results can have important implications for the design and application of treatments that target phagocyte-mediated inflammation in MS patients.
They suggest that the initial proinflammatory polarization of phagocytes needs to be prevented rather than reversed, researchers note.
Also, “the timing of interventions, at least of those that aim to block overall phagocyte infiltration or activation, is crucial” they wrote. Such interventions are likely beneficial during the formation of lesions, but may be harmful during lesion resolution “when anti-inflammatory phagocytes dominate the infiltrate.”
“Expanding our understanding of how phagocyte phenotypes evolve in vivo can thus help to better define both the therapeutic opportunities and the limitations of targeting phagocyte actions,” researchers concluded.


