FAQs about Gilenya
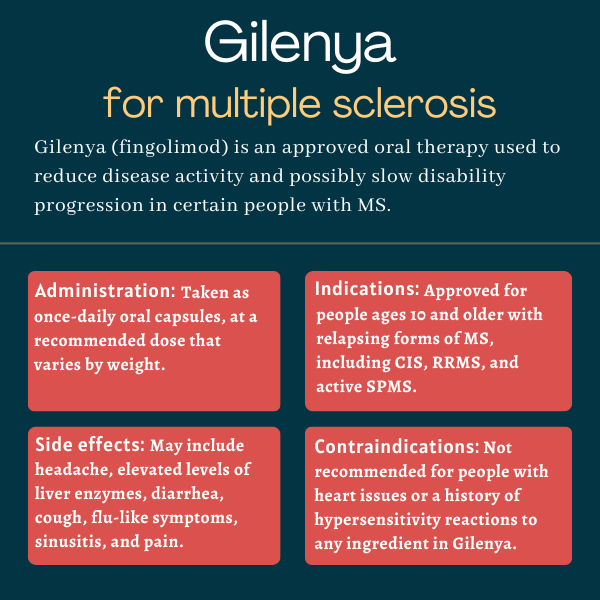
Gilenya was first approved by the U.S. Food and Drug Administration (FDA) in September 2010 for treating adults with relapsing forms of multiple sclerosis (MS), but its label was expanded in 2018 to cover children as young as age 10. In both adults and children, the therapy is approved for clinically isolated syndrome, relapsing-remitting MS, and active secondary progressive MS.
Gilenya has not been well studied in humans during pregnancy, but animal data suggest it may harm a developing fetus. For this reason, patients who have the potential to become pregnant are recommended to use effective contraception while on Gilenya, and for at least two months after stopping treatment.
There is no known interaction between alcohol and Gilenya. However, alcohol can interfere with some medications and exacerbate disease symptoms, so it is recommended that patients talk about this issue with their healthcare providers.
Gilenya quickly lowers the amount of immune cells in circulation, but it could take several months before patients start to notice effects from the medication. As each multiple sclerosis patient is unique, a discussion with their healthcare team can help patients understand how the medication may help in their specific case.
Changes in body weight have not been reported as side effects of Gilenya, but some people who received the medication in clinical trials have experienced hair loss. Patients who experience unanticipated effects of treatment should discuss these with their care team.
 Fact-checked by
Fact-checked by