MS in men: Are there specific MS symptoms for men?
Multiple sclerosis (MS) in men may look different than MS in women. While the condition varies widely from person to person, research has shown that the risk of developing MS in men, as well as disease symptoms, early signs, and long-term outcomes, all tend to differ from those seen in women.
Biological sex and gender identity are separate concepts. This article uses the term “men” to refer to people assigned male at birth, who typically have one X and one Y chromosome and a hormone profile characterized by high testosterone levels.
How common is MS in men?
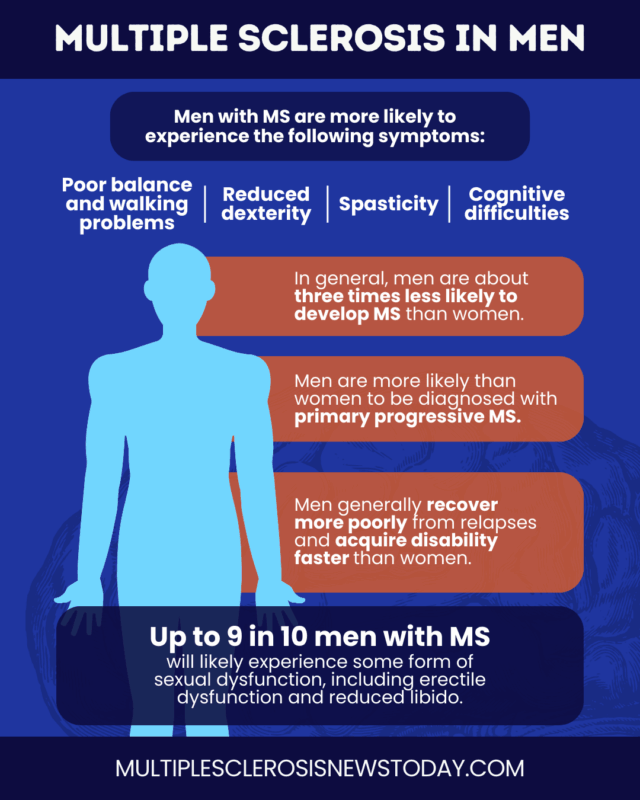
In general, men are about three times less likely to develop MS than women, and the gap between the sexes has widened in the last few decades. In the U.S., recent estimates suggest that MS affects about 450 per 100,000 women and 160 per 100,000 men.
However, MS prevalence in men varies by MS type:
- Relapsing-remitting MS (RRMS), the most common form, which is marked by periods of symptom worsening followed by periods of recovery, is about two to three times more common in women than in men.
- Primary progressive MS (PPMS), a less common form in which symptoms gradually worsen from disease onset, affects men and women at almost equal rates.
Are there specific MS symptoms in men?
While men with MS do not usually experience unique symptoms, research suggests there are some differences in MS symptoms between men and women.
For example, men are more likely to be diagnosed with PPMS, so MS symptoms in men more often present with a progressive course from disease onset.
Men are also more likely to experience symptoms such as:
- poor balance and walking problems
- reduced finger dexterity
- spasticity, or muscle tightness and spasms
- cognitive difficulties
Some of these neurological symptoms of MS in men are also more severe or progress faster than in women. In contrast, pain, mental health issues, and fatigue tend to be more common in women with MS.
Other aspects of MS that may look different in men include:
- Early signs of MS: Women more often present with depression, sensory changes, or vision problems, while common first signs of MS in men more often involve muscle weakness and other motor symptoms.
- Relapse recovery: Among people with relapsing forms of MS, men tend to have fewer relapses but recover more poorly from them, more often showing lingering symptoms between attacks.
- Neurodegeneration: Men tend to have higher rates of brain volume loss and more lesions with irreversible nerve cell damage, which may contribute to differences in long-term neurological symptoms of MS in men.
- Disability accumulation: Disability progression in men with MS is typically faster, causing men to reach certain disability milestones earlier than women. Men with RRMS also tend to transition to secondary progressive MS somewhat earlier than women.
Why is MS different in men?
Sex-related differences in MS are thought to arise from a combination of biological and environmental factors. These may act as risk factors for MS in men or contribute to differences in how MS affects men and women.
- Sex hormones: Differences in testosterone and estrogen levels can influence immune activity and nerve cell health. Before puberty, when hormonal differences are less pronounced, MS occurs at similar rates in boys and girls.
- Immune system: Women generally have stronger immune responses, which increase their susceptibility to autoimmune diseases such as MS.
- Genetics: Certain genetic risk factors can also make women more susceptible to autoimmunity, while others may contribute to the greater neurodegenerative burden and faster MS progression in men.
- Environmental exposures: Factors such as smoking or use of hormonal contraceptives may differ in men and women and can influence MS risk and outcomes.
Common MS experiences in men
The manifestations of MS are unique for each individual, but men can face unique social and psychological challenges that can make coping with MS more challenging.
Disability and masculinity
Among people with similar levels of disability, men tend to rate their physical, psychological, and social well‑being more negatively than women, and report a greater impact on quality of life.
Several factors could help explain this difference. MS can disrupt the common cultural narrative of men as protectors and providers, challenging a man’s perception of his own identity.
Aside from MS, men are also generally less likely to seek healthcare services or mental health support that can improve clinical outcomes and day-to-day living.
MS and sexual intimacy
Damage to the nervous system from MS can interfere with sexual function, while symptoms such as fatigue or spasticity and the emotional impact of MS can further affect intimacy. As a result, sexual dysfunction in men with MS is common.
As many as 9 in 10 men with MS experience some form of sexual dysfunction, which may include:
- erectile dysfunction, or problems achieving or maintaining an erection
- reduced libido
- decreased genital sensation
- difficulty reaching orgasm
Men with MS are encouraged to discuss changes in sexual function with their healthcare team and communicate openly with partners to identify strategies or treatments that may help.
Life expectancy and prognosis of men with MS
MS is not a fatal disease, but it can increase the risk of health complications, such as severe infections, which may shorten life expectancy. On average, people with MS live about 5-10 years less than the general population, though this gap is closing as care for MS patients continues to improve.
In the general population, men typically have an overall shorter lifespan than women, and this pattern is also observed in MS. For example, a 2017 study from Norway reported a median lifespan of 72.2 years for men with MS, compared with 77.2 years for women.
Faster disability progression in men with MS may contribute to these differences, as accumulating disability is strongly linked to a worse long-term outlook for men with MS.
Multiple Sclerosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by 

