Immunosuppressive Therapy, Cell Transplantation Offers Promising Treatment for Relapsing-Remitting Multiple Sclerosis
Written by |
 Immunosupressive therapy in combination with hemotopoietic cell transplant was found to induce remission of Multiple Sclerosis activity for up to 3 years. The new findings could usher in a new mode of effective treatment for MS that could greatly improve quality of life for those with the disease and extend asymptomatic periods.
Immunosupressive therapy in combination with hemotopoietic cell transplant was found to induce remission of Multiple Sclerosis activity for up to 3 years. The new findings could usher in a new mode of effective treatment for MS that could greatly improve quality of life for those with the disease and extend asymptomatic periods.
The study, entitled “High-Dose Immunosuppressive Therapy and Autologous Hematopoietic Cell Transplantation for Relapsing-Remitting Multiple Sclerosis (HALT-MS): A 3-Year Interim Report,” was recently published in the journal JAMA Neurology.
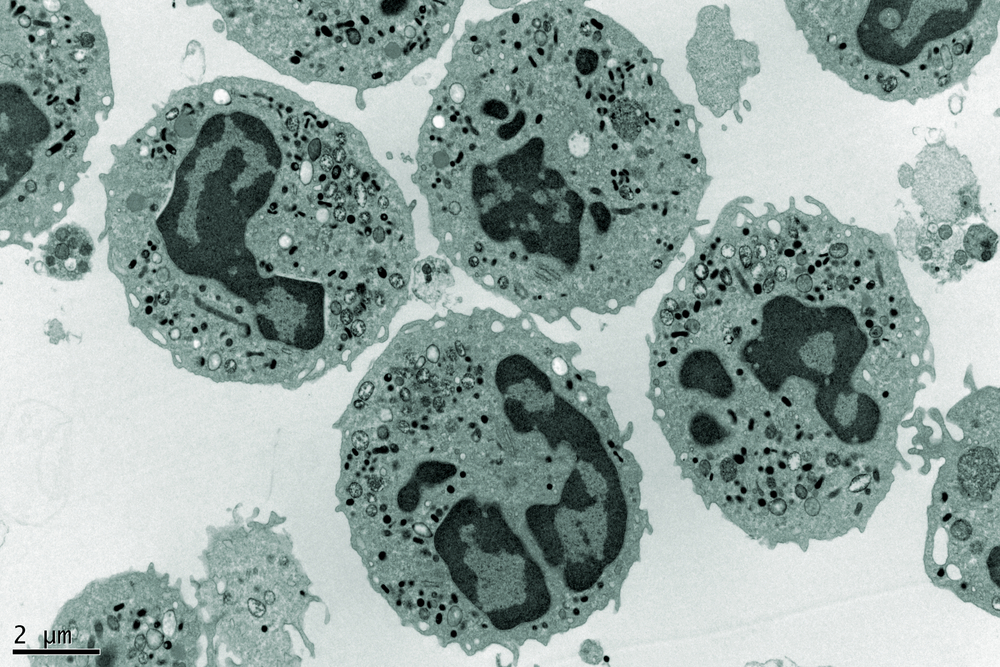
Multiple sclerosis (MS) is an autoimmune condition that causes migration of immune cells to the central nervous system, production of proinflammatory cytokines, demyelination, and neuronal damage. Active inflammation is most evident in early relapsing-remitting (RR) MS.
Autologous hematopoietic cell transplant (HCT) has been tested with the goal of removing disease-causing immune cells and inducing reset of the immune system in patients with advanced disabilities and progressive forms of MS.
[adrotate group=”4″]
Clinical trials of high-dose immunosuppressive therapy (HDIT)/HCT showed that patients with active central nervous system inflammation before HDIT/HCT had a significantly better outcome compared with those without active inflammation before HDIT/HCT. In this regard, the team of researchers led by Richard A. Nash, MD, from the Colorado Blood Cancer Institute in Denver assessed the safety, efficacy, and durability of MS disease stabilization through 3 years after HDIT/HCT in the early inflammatory stage of MS (RRMS).
The Hematopoietic Cell Transplantation for Relapsing-Remitting Multiple Sclerosis (HALT-MS) is a phase 2 study investigating the efficacy of early intervention with HDIT/HCT for patients with RRMS and breakthrough disease. The trial’s primary end-point was event-free survival that involved survival without death or confirmed loss of neurologic function, clinical relapse, or new lesions observed on magnetic resonance imaging.
A total of 25 RRMS patients were eligible and evaluated through 5 years after HCT. However, this study only reported a 3-year interim analysis. From these, 24 received HDIT/HCT. At 3 years, overall event-free survival was 78.4%, progression-free survival was 90.9% and clinical relapse-free survival was 86.3%. No major toxic effects were observable. HDIT/HCT without maintenance therapy was effective for inducing sustained remission of active RRMS and was associated with improvements in neurologic function.
These findings offer an encouraging therapeutic option for MS patients who are unable to receive conventional immunotherapy, since HDIT/HCT was able to induce remission for up to 3 years in most of the patients. However, a longer follow-up period is necessary to determine the durability of the response. Results from the HALT-MS trial will produce a 5-year observation.


