Study Identifies Blood Coagulation Protein Fibrinogen as Cause of Brain Autoimmunity
Written by |
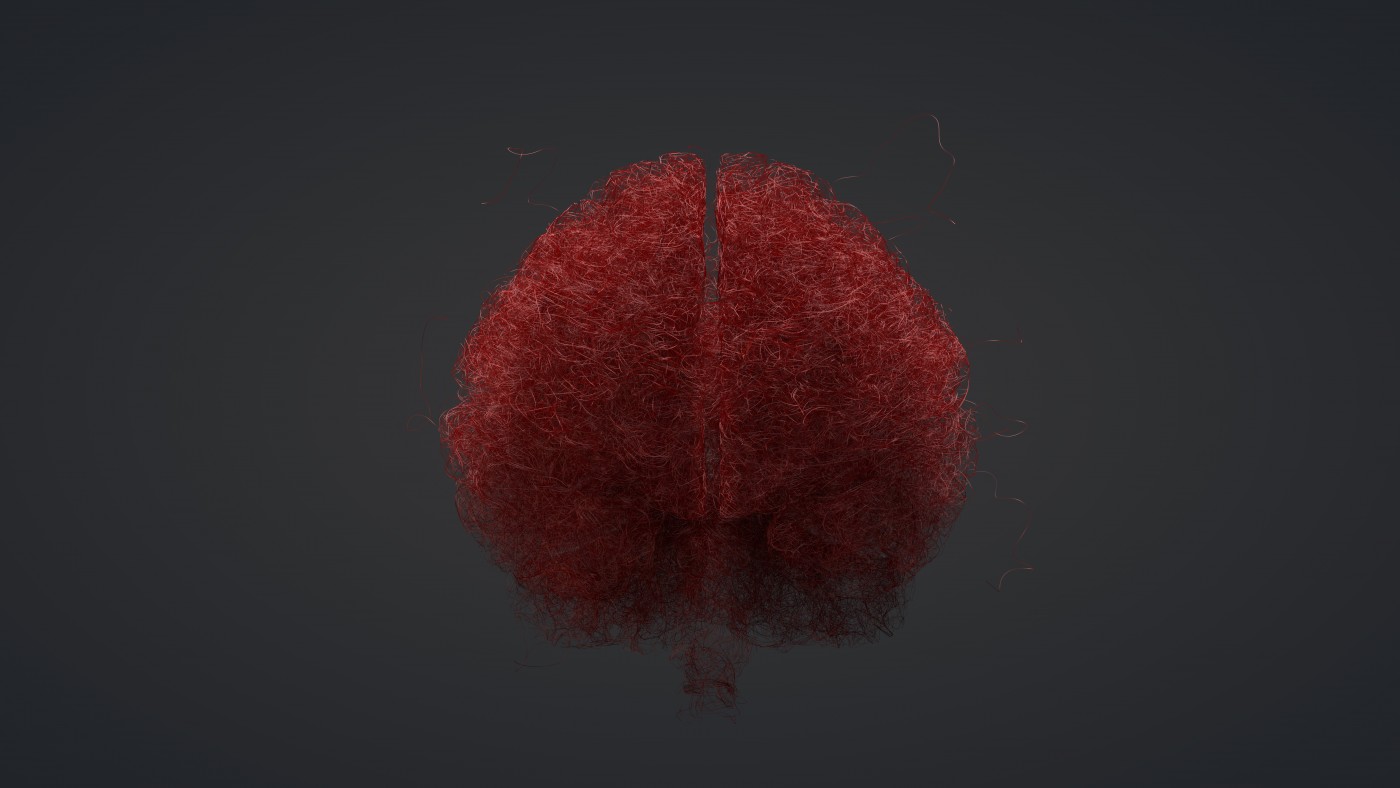
Researchers from the Gladstone Institutes have shown in a new study that fibrinogen, an important blood coagulation protein, can induce an autoimmune response in the central nervous system when the blood-brain barrier (BBB) is disrupted and blood proteins enter the brain. The study, entitled “Blood coagulation protein fibrinogen promotes autoimmunity and demyelination via chemokine release and antigen presentation”, was published in the journal Nature Communications.
Autoimmunity responses and recruitment of immune cells, such as macrophages and T cells, to the brain are events critical to the pathogenesis of neuroinflammatory diseases such as multiple sclerosis (MS). The mechanisms of autoimmunity in the brain are, however, still unclear.
In this study, researchers showed that leakage of blood into the brain leads to analogous responses to those observed in MS. To achieve these conclusions, researchers developed a new animal model in which blood was injected into the brain, resulting in a cascade of events leading to autoimmunity, inflammation and demyelination, a key factor in MS. Myelin is a protective layer that covers nerves in the brain. Researchers were also able to specifically identify the blood component triggering this response, the blood clotting protein fibrinogen.
The team hypothesized that the presence of fibrinogen in the brain would activate microglia (brain’s immune cells), which in turn would recruit macrophages and T cells which cause damage to the myelin layer. In order to confirm fibrinogen’s central role in the autoimmune response, the scientists deleted fibrinogen’s receptor on microglia. This deletion resulted in an absence of immune response, and stopped myelin damage and brain inflammation.
First author Jae Kyu Ryu, PhD, a staff research scientist at the Gladstone Institutes, commented on these results in a news release: “Our results provide the first evidence that blood promotes T cell responses against the brain. Not only did we confirm that the presence of blood in the brain recruits peripheral immune cells to the area, which is sufficient to cause myelin destruction, we also identified fibrinogen as the critical protein driving this process.”
Future research includes finding new molecules to block fibrinogen activity and suppress autoimmunity in the brain. Besides contributing to the development of potential new MS therapies, this research enlightened the cause-effect mechanism of brain damage and immune response, as stated by the study’s senior co-author Scott Zamvil, MD, professor of neurology at the University of California, San Francisco, “These findings question a long-held paradigm that myelin-specific T cells initiate inflammation in the brain through activation of microglia and brain macrophages. This study demonstrates that the original paradigm may also occur in reverse. Namely, initial activation of microglia and brain macrophages may activate T cells.”


