Woman with PML Linked to MS Therapy Successfully Treated with IL-2 Cytokine
Written by |
A case report of a woman with relapsing-remitting multiple sclerosis (MS), who developed progressive multifocal leukoencephalopathy (PML) after natalizumab therapy, found that the immune-boosting molecule interleukin-2 (IL-2) might be a viable therapeutic option to fight this life-threatening complication although further study is needed.
The case report, “Use of interleukin-2 for management of natalizumab-associated progressive multifocal leukoencephalopathy: case report and review of literature,“ was published in the journal Therapeutic Advances in Neurological Disorders.
PML, caused by the John Cunningham (JC) virus, is a rare but serious condition, the consequence of the treatment with natalizumab (Tysabri). Researchers and clinicians have tried various approaches to limit the infection, but none have proved successful so far.
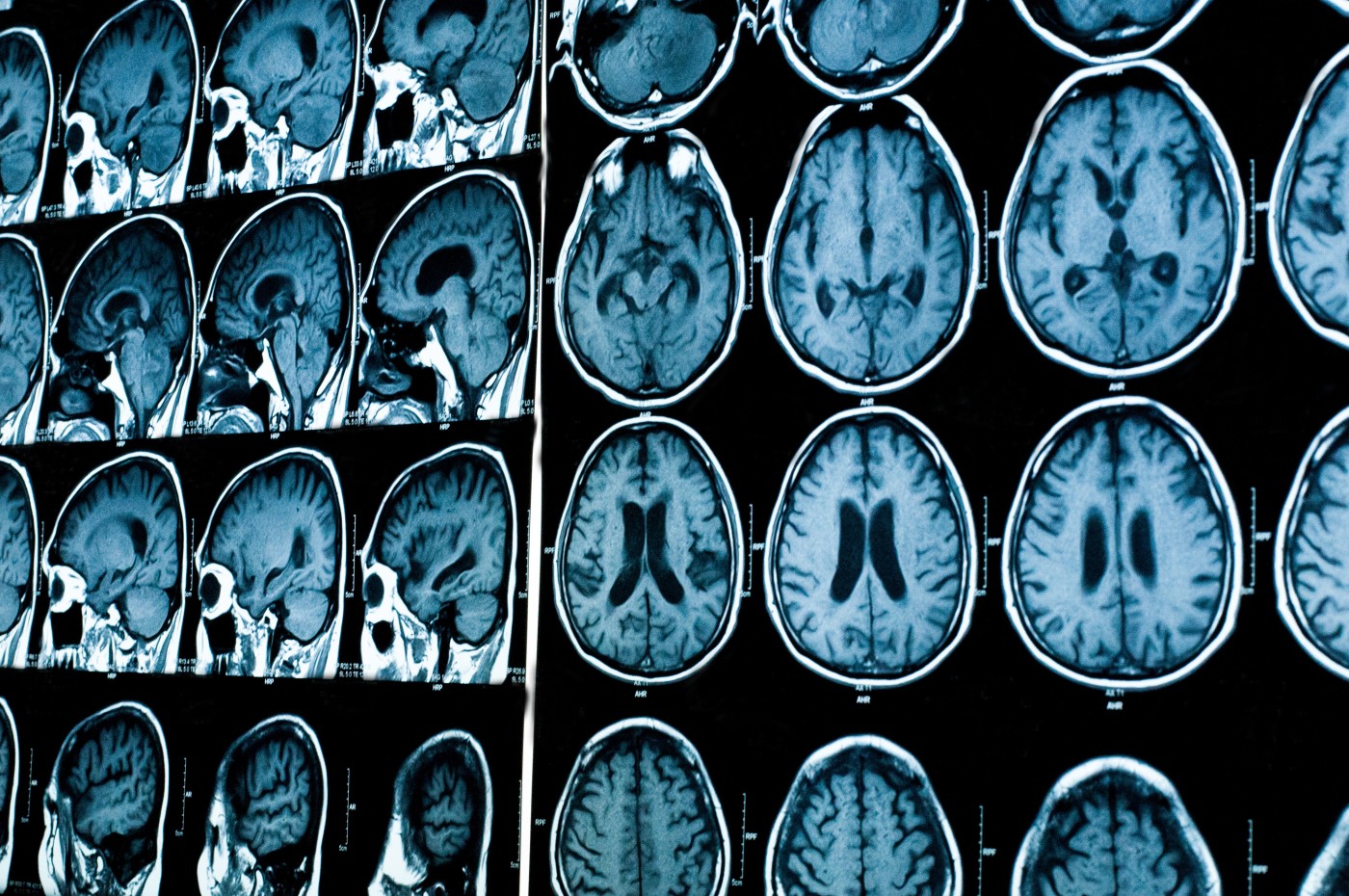
The woman, 51, came to the attention of the clinical research team at UT Southwestern Medical Center when she developed expressive aphasia, the inability to speak, and became weak along the right side of her body. Magnetic resonance imaging (MRI) scans showed new brain lesions, and she tested positive for the JC virus. Her condition worsened despite plasmapheresis and immunoglobulin treatment, and she developed epileptic brain activity.
High levels of the virus were found in her cerebrospinal fluid, and the team started treating her with IL-2. The IL-2 cytokine triggers the development of cytotoxic T-cells that fight the virus, and has been used to treat PML in patients with blood cancers. Treatment with IL-2 may increase the risk of MS progression, but the research team deemed it to be a much lower risk than the potentially fatal consequences of PML.
When discontinuing natalizumab treatment, patients are at risk of developing what is known as immune reconstitution inflammatory syndrome (IRIS). This happens when the immune system starts to recover because an immunosuppressive or modulating therapy has been stopped, and reacts to a present infection so robustly it makes the symptoms worse. Since the boosting of T-cells by IL-2 might further increase the risk of IRIS, the woman also received high-dose corticosteroids to dampen inflammatory reactions.
Results showed that the woman gradually improved on the IL-2 therapy. Her speech returned and she regained muscle strength — features that were accompanied by lower virus levels and a disappearance of MRI lesions. She did not experience any severe side effects of the IL-2 treatment.
The authors concluded, however, that more studies are needed to explore the benefit of this treatment in MS patients who develop PML.


