#ECTRIMS2016 – Brain MRI Scans Can Predict Which Patients Will Progress into SPMS
The presence of certain brain and spinal cord lesions can be used to predict if an MS patient with clinically isolated syndrome will progress into relapsing or secondary progressive multiple sclerosis (SPMS) within 15 years.
Researchers agree that knowing which patients who will rapidly deteriorate will help physicians tailor both monitoring and treatment according to these patients’ needs.
The study, “Early MRI predictors of secondary progressive multiple sclerosis: a 15 year follow-up study of patients with clinically isolated syndrome,” was presented at the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS) 2016 Congress Sept. 14-17 in London, where MS researchers presented their latest findings.
The presentation was titled “Long term outcome after presentation with a clinically isolated syndrome,” and was given by Wallace Brownlee from the Queen Square Multiple Sclerosis Centre at University College London.
Brownlee described how earlier studies had identified patient characteristics linked to a faster disease development among relapsing MS patients. The studies found that age, sex, the type of symptoms and the recovery from the first attack could all be used to predict if a patient would have an early transition from clinically isolated syndrome to SPMS.
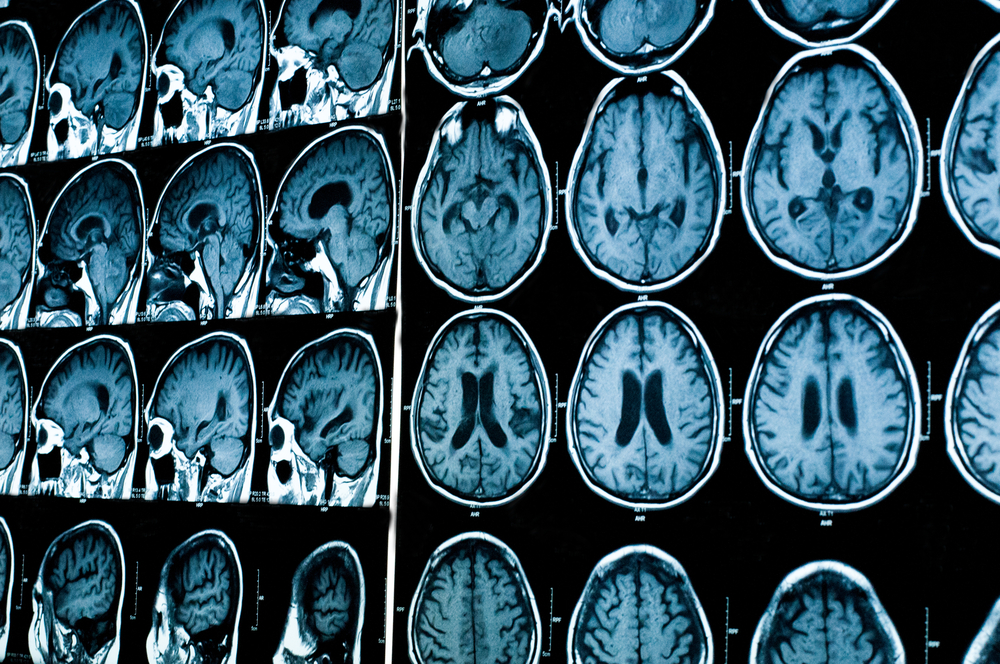
To strengthen the predictions, Brownlee and colleagues explored whether magnetic resonance imaging (MRI) of the brain and spinal cord at the first neurological MS-type episode, known as clinically isolated syndrome, could predict the disease course.
The team studied 164 patients who had different kind of MRI measurements, including the load, activity, and placement of lesions, as well as measures of neurodegeneration.
Patients were assessed 15 years later, and the study showed that 27 percent remained classified as clinically isolated syndrome; another 58 percent had developed relapsing MS; and 15 percent had progressed to SPMS.
Researchers noted that the presence of certain types of lesions during the first episode could predict an early transition to secondary progressive MS. Data also indicated that a larger loss of neurons in white matter lesions may drive disease progression and contribute to the development of SPMS.
“In patients with CIS [clinically isolated syndrome], spinal cord, infratentorial and non-enhancing T1-hypointense brain lesions are associated with a higher probability of SPMS , rather than RRMS [relapsing-remitting multiple sclerosis] or CIS after 15 years.
“These findings suggest that lesions in clinically-eloquent sites and a greater extent of neuroaxonal loss within brain white matter lesions may be potential mechanisms that contribute to the development of SPMS,” the team wrote in their ECTRIMS abstract.






