Potential Mechanism Behind Effectiveness of B-cell Depletion Therapy in MS Uncovered
Written by |
The loss of immune B-cells, and the resulting changes in the profile of immune T-cells, is a major mechanism of action for the beneficial effects seen with ublituximab treatment in multiple sclerosis (MS) patients, a study suggests.
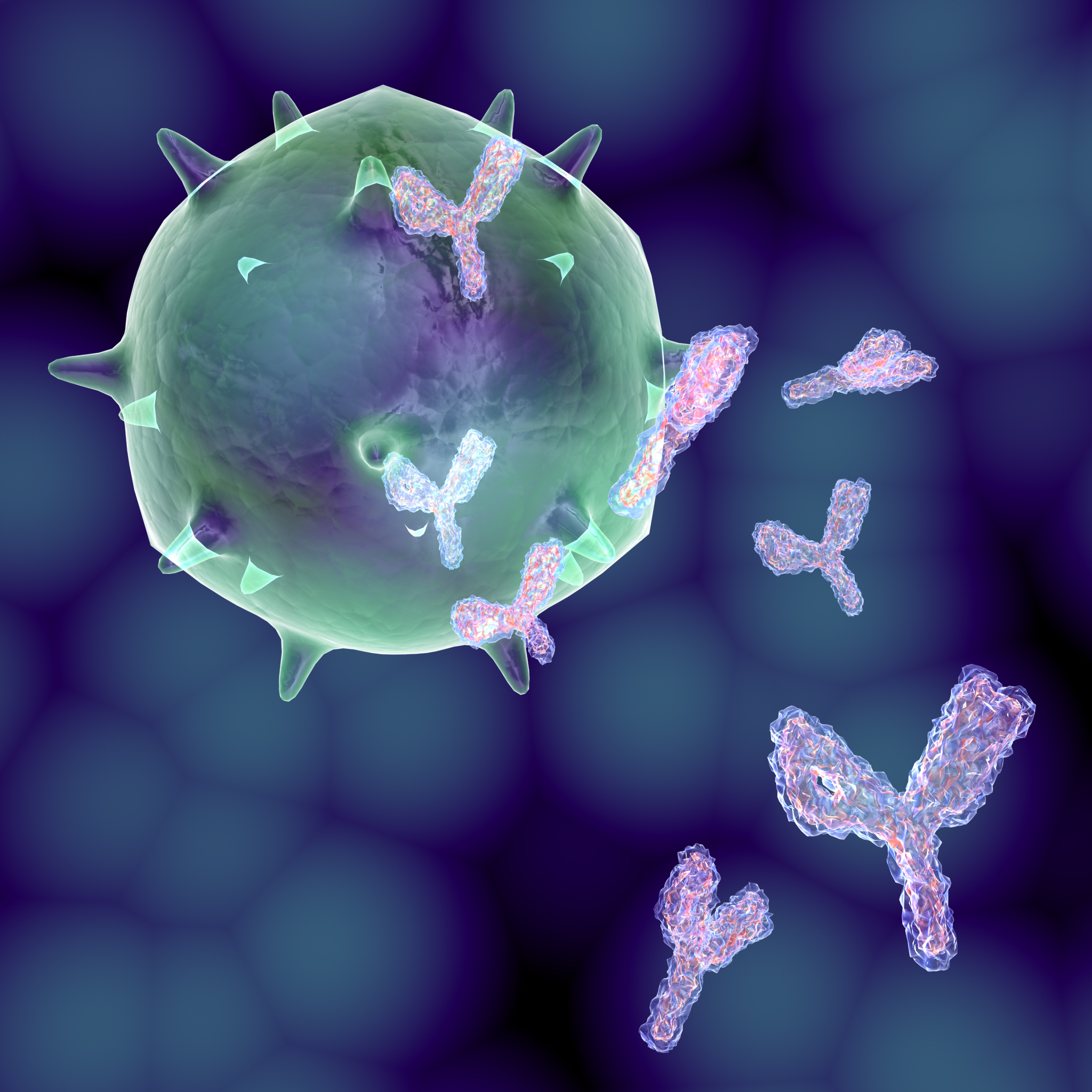
B-cells are a type of immune cell best known for producing antibodies. Therapies that decrease the number of B-cells are effective for some people with MS — but therapies that only decrease patients’ antibody levels aren’t. This raises the question of why depleting an MS patient’s B-cells is therapeutic if it’s not because of decreased antibodies.
The study, titled “B cell depletion with ublituximab reshapes the T cell profile in multiple sclerosis patients,” suggests that this effect may be due to changes in other types of immune cells with which B-cells interact, namely T-cells. It was published in the Journal of Neuroimmunology.
A total of 48 people with relapsing MS (32 females; average age of 39.2 years) were recruited for a Phase 2a clinical trial (NCT02738775) testing ublituximab (TG-1101), an investigational monoclonal antibody being developed by TG Therapeutics.
By targeting CD20, a protein on B-cells, ublituximab can significantly decrease the number of B-cells. Importantly, because of how CD20 is expressed, ublituximab does not have much of an effect on mature B-cells that are already making antibodies, called plasma cells.
Enrolled MS patients were given two infusions of ublituximab three weeks apart. Blood samples were taken before the first infusion, and several times over the next 24 weeks. Samples were then analyzed to determine the type of immune cells present.
Researchers first confirmed that ublituximab treatment did in fact reduce the number of B-cells in patients, which remained low throughout the study period. They then looked at how this change — the depletion of B-cells — affected other types of immune cells.
First, the team noticed that, after B-cell depletion, there was a rapid rise in the number of myeloid cells compared with other types of immune cells, especially T-cells and natural killer cells. Myeloid cells are a class of immune cells that include some of the “first responders” against possible threats, such as infections, so the researchers think this increase might be the body trying to quickly compensate for the lack of B-cells.
More striking, the researchers observed a change in patients’ T-cell profile. T-cells are part of the adaptive immune system, which means that individual T-cells can specifically recognize a particular molecular pattern, called an antigen, such as a protein from a particular bacteria or virus. Before a T-cell “sees” the specific antigen it recognizes, it can be considered a “naive” T-cell.
Memory T-cells, in contrast, are descendant from T-cells that have reacted to an antigen and induced an immune response. These memory cells hang around in the body so that, if the same antigen is encountered again, they can activate a powerful defense response very quickly.
Researchers found that, after patients were treated with ublituximab, they had far fewer memory T-cells relative to naive T-cells. Additionally, these patients had more of a subset of T-cells called regulatory T-cells (Tregs, which help “put the brakes” on the immune system, reducing inflammation) compared with Th1 cells, a type of T-cell that secretes proinflammatory signal molecules.
“B-cell depletion in MS patients reduces memory T-cells and increases naïve T-cells, suggesting that T-cell activation is reduced when B-cells are low,” the researchers wrote.
Overall, the data indicate a generally smaller inflammatory T-cell population in MS patients who had undergone B-cell depletion through ublituximab treatment. This observation may provide the answer to how this B-cell depletion has a therapeutic effect in MS patients.
The team believes that the change in T-cell profile is what makes B-cell depletion an effective strategy in MS.
“The change in T-cell subsets following B-cell depletion observed in this study suggests that B-cells are important APCs [antigen presenting cells ] in MS, and depletion of B-cells reduces T-cell activation and shifts the balance of naïve, effector and memory T-cells,” they concluded.


