Early MRI Findings May Predict Disease Worsening in Children with MS
Written by |
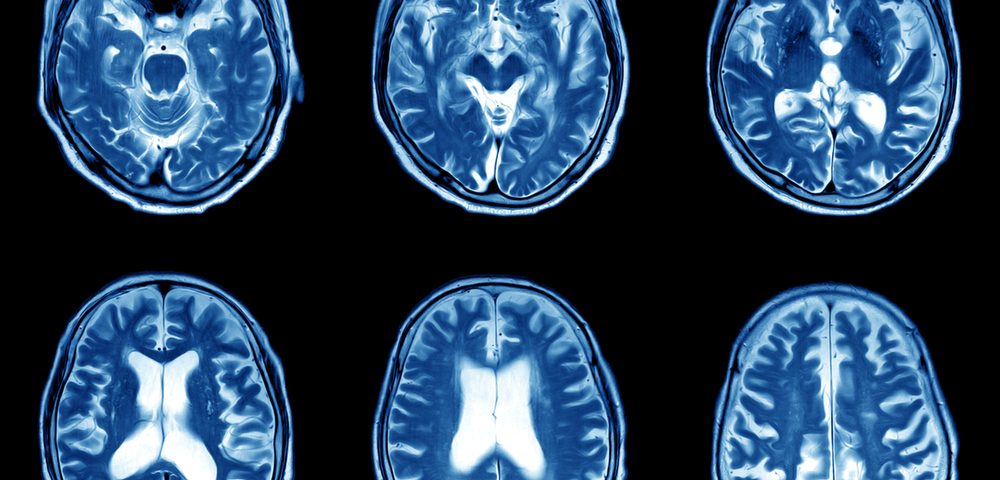
Abnormalities detected on MRI scans at the onset and within the first two years of disease may predict disability worsening in children with multiple sclerosis (MS), a nine-year study reports.
Specifically, damage in the spinal cord, brain, and optic nerve plays a major role in predicting outcomes in these patients, underscoring the need for comprehensive imaging tests early on, researchers say. They found that children with MS exposed to high-efficacy disease-modifying treatments (DMTs) in the first year of disease had lower disease activity in the nine-year follow-up.
The study, titled “Early Predictors of 9-Year Disability in Pediatric Multiple Sclerosis,” was published in the Annals of Neurology.
MS is characterized by the loss of the myelin sheath, or fatty protective coating, that covers nerve fibers. This myelin loss results in MS lesions on the brain or spinal cord that can be identified through imaging tools such as MRI.
In adult MS patients, MRI lesions have been shown to be linked to the development of clinical disability within five to seven years after the first clinical signs of disease.
In children, MS is typically characterized by higher levels of clinical activity, relapse rate, and MRI activity, compared with adult-onset MS. “However, little is known about how these early clinical and MRI features may influence the long-term clinical outcome of these patients,” the researchers wrote.
Furthermore, given the small number of approved DMTs for pediatric MS, “it appears extremely relevant to identify risk factors for disease progression in these patients,” the team added.
Therefore, the researchers analyzed a group of pediatric MS patients to identify early clinical and MRI predictors of disease course.
In total, 123 children (89 girls and 34 boys, average age of 14.4 years), with relapsing-remitting MS, followed at San Raffaele Hospital, Milan, Italy, were enrolled in the study.
Data was gathered at disease onset, after one and two years, and at the last clinical visit — the median follow-up duration was 9.4 years. DMT exposure, MRI scans, relapse rate, and disability levels (measured through the Expanded Disability Status Scale, or EDSS, score rating) were assessed.
First, the team tried to identify predictors of the time to first relapse and of the average number of relapses in one year, or annualized relapse rate (ARR).
The time from disease onset to first relapse ranged from 0.2 to 13.7 years, with a median of 1.7 years.
The presence of optic nerve lesions was found to be a predictor of the time to first relapse, with a hazard ratio of 2.10, which means that patients with lesions in the optic nerve were at 2.10 times higher risk of developing a first relapse.
High-efficacy DMT exposure could also independently predict the time to first relapse, with a hazard ratio of 0.31, meaning that treatment reduced the risk of relapses (hazard ratios under one indicate a decreased risk).
Lesions in the cerebellum region of the brain at disease onset and exposure to high-efficacy DMTs were both associated with lower ARR. In contrast, lesions in the spinal cord predicted a higher ARR.
The researchers also found that the higher the number of relapses during the first year of disease, the higher the ARR would be.
“ARR over the first 9 years of disease, was in part predicted by baseline lesion distribution,” the researchers wrote. “In details, cerebellar lesions were associated with lower ARR, whereas cervical cord lesions were associated with higher ARR.”
The team then assessed disability worsening over the nine-year follow-up.
In this period, 13 (11%) out of the 123 pediatric patients experienced disability worsening. Patients whose disease worsened had a higher number of new brain MRI lesions and greater EDSS change at one and two years after disease onset, compared with patients who did not experience disease worsening.
More specifically, the presence at MS onset of optic nerve lesions was associated with a higher probability of nine-year disability worsening — odds ratio (OR) of 6.45, meaning a 6.45 higher chance compared to patients without lesions in the optic nerve.
Furthermore, EDSS changes during the first two years of disease (OR of 16.38), as well as the presence of at least two new brain T2 MRI lesions (OR of 4.91) were also associated with an increased probability of nine-year disability worsening. T2 MRI lesions represent the total lesion load (with and without active inflammation).
Next, the researchers looked at factors that could predict the EDSS score at nine years after MS onset. Of note, a higher EDSS score indicates greater disability.
They found that the EDSS score, the presence of brain lesions, and the number of spinal cord lesions at MS onset were predictors of a higher nine-year EDSS score.
At one or two years after MS onset, an EDSS change and two or more new T2 lesions were associated with higher EDSS scores at nine years.
Overall, “a complete baseline MRI assessment and an accurate clinical and MRI monitoring during the first 2 years of disease contribute to predict 9‐year prognosis in pediatric patients with multiple sclerosis,” researchers wrote.
“High-efficacy DMT exposure over the first year of disease reduced disease activity over the 9-year follow-up,” the team concluded. “Baseline cervical cord, brainstem, and optic nerve involvement by lesions have a major role in predicting 9-year outcomes, both in term of disease activity and disability worsening, underscoring the need for complete CNS [central nervous system comprising the brain and spinal cord] MRI assessment at baseline.”


