Chronic Inflammation in MS Linked to Specific Brain Cells in Study
Written by |
An interaction between immune cells and glia cells in the brain, mediated by the C1q complement system protein, appears to drive chronic inflammation in multiple sclerosis (MS), new research shows.
Inhibiting this protein helped to resolve inflammation in mouse models of MS and in tissue cultures, its researchers found. Understanding these interactions further may pave the way to new treatment approaches, including ones that might be relevant to progressive MS.
The study “A lymphocyte–microglia–astrocyte axis in chronic active multiple sclerosis” was published in Nature.
MS is caused by inflammation that damages the brain, particularly the fatty myelin coating surrounding nerve fibers. The exact biological mechanisms that drive this inflammation are incompletely understood, which has posed a stumbling block for the development of treatments.
“We have terrific therapies that block new inflammation but nothing to stop the inflammation that’s already there. In order to make strides in developing new therapies for progressive MS, we’re going to need to pick apart the cellular and molecular mechanisms one by one,” Daniel Reich, MD, PhD, a researcher at the National Institute of Neurological Disorders and Stroke and the study’s co-senior author, said in a press release.
Researchers performed a detailed analysis of brain lesions with a particular feature visible on MRI scans: inflamed rims, or “smoldering” plaques. These areas of the brain are thought to be where chronically active inflammation is taking place in MS.
The researchers combined detailed dissections of brain tissue with a technology called single-nucleus RNA sequencing to examine the transcriptomes of cells in these plaques. The transcriptome is essentially a global view of gene expression — that is, which genes are “turned on” or “turned off” within a given cell.
“Our dataset is very rich. The beauty of having such a detailed map is that now we have a better understanding of the entire network of cells involved in smoldering inflammation,” said Martina Absinta, MD, PhD, a professor at Johns Hopkins University and study author.
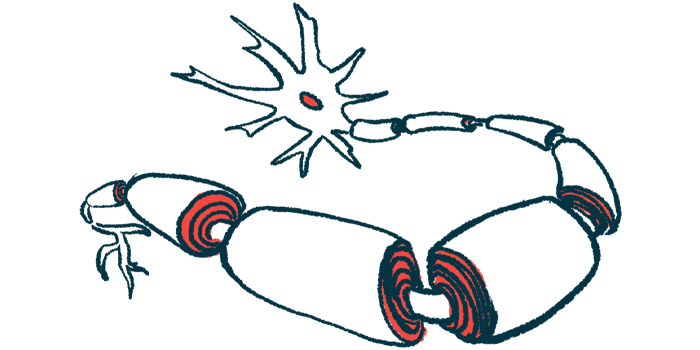
By analyzing the different cell types and their gene expressions, the researchers were able to gain insight into the probable interactions between the different cells, and how they likely contribute to inflammation. In particular, they found evidence for interactions between lymphocytes — immune cells like B-cells and T-cells — and certain cells in the brain called glia.
Glia are a non-neuron class of brain cells — they don’t send electrical signals, but perform a variety of other functions needed to keep the brain healthy. The researchers’ findings specifically implicated two kinds of glia called microglia and astrocytes.
Among astrocytes’ various functions in the brain is helping to maintain the health of synapses (connections between nerve cells). Microglia are specialized cells that help to protect the brain against infections.
In MS lesions, both astrocytes and microglia had characteristic pro-inflammatory gene expression profiles, likely contributing to disease progression in MS, the researchers wrote.
Further investigation in mouse models and tissue cultures suggested that these cells’ inflammatory state was largely driven by activation of the complement system, a group of blood proteins that normally act as part of the immune system’s response to infection.
Specifically, the researchers showed that a complement protein called C1q plays a central role in driving the inflammatory activity of the brain cells, and that genetically engineering mice to lack this protein in microglial cells, or by blocking C1q in tissue samples largely attenuated chronic inflammation.
This suggests that “pharmacological inhibition of C1q is a potential therapeutic avenue towards addressing chronic inflammation” in MS, the researchers wrote.
“These results give us a way to test new therapies that might speed up the brain’s healing process and prevent brain damage that occurs over time,” Reich said. Earlier work by Reich and his team noted chronic active lesions, identified on MRI by their darkened outer rims, as a possible hallmark of progressive MS forms.
Assessing these lesions via MRI scans may be useful as a marker of disease progression or therapy efficacy in MS clinical trials, the team added, providing some early analyses that could support using these lesions as biomarkers for those purposes.
